Home ►
SPOT UG 3 Eligibility
Last Modified: 5/29/2025
Location: FL, PR, USVI
Business: Part A, Part B
Eligibility
SPOT interfaces with the CMS HIPAA Eligibility Transaction System (HETS) to obtain eligibility information. HETS is considered the authoritative source for beneficiary information. Per CMS, “The HIPAA Eligibility Transaction System (HETS) is intended to allow the release of eligibility data to Medicare providers or their authorized billing agents for the purpose of preparing an accurate Medicare claim, determining beneficiary liability, or determining eligibility for specific services.” More information about HETS can be found at
https://www.cms.gov/Research-Statistics-Data-and-Systems/CMS-Information-Technology/HETSHelp/index.html.
Eligibility information is available 24/7 (excluding holidays and scheduled maintenance periods). The display and accessibility of specific Eligibility tab submenu options (e.g., Hospice / Home Health, MSP) are contingent upon the availability of active data directly associated with the beneficiary and each submenu option.
Eligibility queries are limited to 24 months in the past and four months in the future, based upon date of the query.
If an inactive period is returned but a termination date for either Part A or Part B eligibility is not, it means that the Social Security Administration (SSA) still considers the beneficiary to be entitled to Medicare. However, during the specified inactive period, services furnished to that beneficiary will not be covered.
A few reasons this may happen is when a beneficiary was classified as an illegal alien in the United States, deported from the United States, or incarcerated. Information specifying the reason for the period of ineligibility will not be available in SPOT because it is not released by the HIPAA Eligibility Transaction System (HETS), which is the source for all eligibility data accessed through the SPOT.
Medicare Diabetes Prevention Program (MDPP) providers enrolled with specialty D1 will have access to the following eligibility information (as applicable for the Medicare Beneficiary):
• Medicare Beneficiary Demographics
• Date of Death
• Unlawful Occurrences
• Medicare Part B Entitlement
• MDPP Coverage
• ESRD - Medicare Beneficiaries in an active ESRD occurrence are not MDPP eligible.
• Medicare Advantage (MA) Enrollment(s) - Contact the MA plan for MDPP Coverage Information.
• Medicare as a Secondary Payer (MSP) Enrollment
Eligibility
To utilize the Eligibility feature, the user should take the following steps:
1. Select Eligibility from the top menu.
Figure 1: Eligibility menu
2. Select Eligibility from the drop down menu.
Figure 2: Check Eligibility page
3. Using the search tab on the left, complete the required fields. Scroll to see all available fields.
• Beneficiary Last Name
• Medicare Beneficiary ID
• Beneficiary First Name and / or Beneficiary Date of Birth
• Date(s) of Service.
The current date will be displayed by default.
You may limit your query to the date(s) the service will be furnished to the patient, or you may specify any time up to four months in the future and 24 months in the past.
Figure 3: Eligibility search
4. Click Search to view Eligibility results.
5. If necessary, click the PDF icon for a printer-friendly eligibility report in PDF format.
Figure 4: PDF icon
• Remove the check from any tabs you do not want included on the report by clicking the appropriate box(es) and then click Download PDF to view/print the report. A message will display briefly indicating that your report was downloaded. Go to your internet browser's download location to view the report.
Figure 5: PDF icon
6. Select any of the Eligibility submenu options displayed to view the corresponding information. Only the submenu options that contain active data will be accessible.
Helpful tips:
• Click the arrow

before the word instructions to minimize or expand the instructions.
• Each section of the SPOT Eligibility Report focuses on a different benefits category and includes the beneficiary’s information, the dates of service queried, and all the data returned by the query. You may then save the report or print a copy to place in the patient’s file for easy reference.
• Click the search tab

available on the left side to easily edit your query.
• Depending on your screen display and zoom settings, you may need to scroll to see all fields.
• Hover over the information circle

for code descriptions.
Figure 6: Eligibility / Benefits Inquiry Results
The Eligibility results will include the following information:
• Beneficiary’s information:
• Name
• Date of Birth
• Date of Death (when applicable)
• Date of service
• Address
• Beneficiary’s eligibility/benefits information:
Reminder: Information only appears when applicable to the beneficiary.
• Part A Eligibility: Effective Date - date indicating when the beneficiary first became eligible for Medicare Part A benefits.
• Part A Eligibility: Termination Date - date that indicates the termination of eligibility for Medicare Part A benefits. No date in this field means Medicare Part A eligibility has not been terminated.
• Part A Eligibility: Message – displays the reason a beneficiary is insured with Medicare.
• Part B Eligibility: Effective Date – the date indicating when the beneficiary first became eligible for Medicare Part B benefits.
• Part B Eligibility: Termination Date - date that indicates the termination of eligibility for Medicare Part B benefits. No date in this field means Medicare Part B eligibility has not been terminated.
• Part B Eligibility: Message – displays the reason a beneficiary is insured with Medicare.
• Part B Acupuncture Benefit information.
• Inactive Periods - if data appears in the Inactive Periods section, it means that although the beneficiary is entitled to Medicare, he or she is ineligible for Medicare benefits over the specified period for one or more of the following reasons:
• The Medicare beneficiary has been classified as an illegal alien in the United States.
• The Medicare beneficiary has been deported from the United States.
• The Medicare beneficiary has been incarcerated.
Information specifying the reason for the period of ineligibility will not be released by HETS.
• QMB Enrollment – effective date, termination date, and plan
• Medicare Diabetes Prevention Program (MDPP) (effective date, termination date and period two end date)
• Inactive Medicare Diabetes Prevention Program (MDPP) Periods (effective date and termination date)
• End State Renal Disease (effective date, termination date, dialysis start date, dialysis end date, transplant effective date)
Figure 7: Deductible/Caps Results
The Deductible / Caps results will include the following information:
• Deductible
• Line of business
• Deductible year
• Base amount
• Remaining deductible
• Part B Plan Coinsurance
• Deductible year
• Coinsurance %
• Free services
• Line of business
• Deductible year
• Base amount
• Remaining deductible
• Part B plan coinsurance
• Deductible year
• Coinsurance %
• Part B plan coinsurance free
• Deductible year
• Coinsurance %
• Blood deductible
• Deductible year
• Number of units remaining
• Outpatient mental coinsurance
• Calendar year
• Coinsurance %
• Therapy cap
• Type
• Calendar year
• Used amount
• Rehabilitation sessions
• Type
• Sessions used technical
• Sessions used professional
Figure 8: Preventive Information / History
Preventive services are described by the Healthcare Common Procedure Coding System (HCPCS) and in some cases, Current Procedural Technology (CPT) codes. A
lthough there are many HCPCS and CPT codes for which Medicare provides payment, the following is a listing of the preventive categories currently returned by HETS:
• Alcohol Misuse Screening
• Annual Depression Screening
• Annual Wellness Visit (AWV)
• Behavioral Counseling for Alcohol Misuse
• Behavioral Counseling for Obesity
• Bone Density Measurements
• Cardiovascular Disease Screening (CARD)
• Cognitive Services
• Colorectal Cancer Screening (COLO)
• COVID-19 immunization data
• Diabetes Screening Tests (DIAB)
• Fecal Occult Blood Test (FOBT)
• Hepatitis B Antibody Screening
• Hepatitis C Antibody Screening
• High Intensity Behavioral Counseling (HIBC)
• HIV Screening
• Human papillomavirus (HPV) Screening
• Influenza (Flu) Vaccines
• Initial Preventive Physical Examination (IPPE)
• Intensive Behavioral Therapy (IBT) for Cardiovascular Disease
• Intensive Behavioral Therapy for Obesity
• Lung Cancer Screening
• MDPP
• Pharmacogenomic Testing for Warfarin Response (PTWR)
• Pneumococcal Vaccines (PPV)
• Prostate Cancer Screening (PROS)
• Screening Mammography (MAMM)
• Screening Pap Test (PAPT)
• Screening Pelvic Exam (PCBE)
• Smoking Cessation
• Ultrasound Screening for Abdominal Aortic Aneurysm (AAA)
For more information about this topic, please review:
If HETS does not return eligibility data for a particular code, SPOT will be unable to display it. In addition, data on certain codes will only be returned if the beneficiary meets the criteria required (e.g., age, sex, medical condition) for eligibility.
Preventive Services information displays current information only - no information about historical eligibility may be made based on the returned next eligible dates.
The Preventive information/history results page provides HCPCS codes, next professional date, next technical date for technical preventative services, deductible, and coinsurance information associated with covered preventive services.
The Preventive results will include the following information:
• Smoking cessation
• Preventive services
• MDPP with no prior usage - Procedure codes for MDPP services will display when beneficiary has prior MDPP usage. Code G9873 will display for a beneficiary with no prior MDPP usage.
• MDPP with prior usage
• Services with prior usage
• PPV with no prior usage
• COVID-19 immunization
• Influenza (Flu) vaccination
• MDPP services remaining
• Cognitive services
In the Preventive Services details:
• Professional preventive services refer to procedures performed by the physician (e.g., examination, interpretation of test results)
• Technical preventive services refer to procedures that involve screening or the performance of tests (e.g., radiology test, mammography screening).
The Next Professional Date or Next Technical Date associated with a particular procedure code refers to a date that meets one of the following criteria:
• The date that the beneficiary was first eligible to receive the professional or technical preventive service
The date the beneficiary was first eligible to receive a preventive service may correspond to either the beneficiary’s initial Medicare Part A / B eligibility date or the effective date of Medicare’s coverage for the preventive service
• The date that the beneficiary will be next eligible to receive the professional or technical preventive service
• The Next Professional Date and Next Technical Date may be the same date. However, one date may list the date the service was first made available to the beneficiary, and the other may list the date the beneficiary will be next eligible to receive the service.
Annual Wellness Visits (AWV) are covered by Medicare at 12-month intervals, which means that 11 full calendar months must pass after the month in which a beneficiary had received an AWV.
If the patient has not yet had one of the once-in-a-lifetime codes, the procedure code will display with the “Next Technical Date” and “Next Professional Date” dates populated. These dates will indicate the next time the patient is eligible for the service. This date may even be a past date if the patient has already been eligible for that service for some time.
Additionally, certain once-in-a-lifetime codes like the initial Welcome to Medicare visit (which is only eligible within the first 12 months of their Medicare coverage) may still display the procedure code within the search results, but with no “next date” populated. This indicates the patient is no longer eligible for that procedure code.
Some related codes, such as pneumonia vaccinations and boosters, require additional information to determine the patient’s eligibility. If the patient has already had one of the codes, none will display within the preventative tab. This is because the CMS HETS system cannot verify all information required to display the eligibility of subsequent codes.
Medicare Secondary Payer (MSP) Figure 9: MSP Results
The beneficiary's MSP information results will include only active MSP data per the date(s) requested and will not be accessible if there is no MSP data or if notification of coverage primary to Medicare has not been received by CMS.
For each Medicare Secondary Payer (MSP) payer, the following information will be displayed:
• Type of Primary Insurance – the type of insurance provided for the beneficiary, which may fall into any of the following categories:
• Medicare Secondary Working Aged Beneficiary or spouse with Employer Group Health Plan
• Medicare Secondary End-Stage Renal Disease Beneficiary in the 12-month coordination period with an Employer Group Health Plan
• Medicare Secondary No-Fault insurance including auto is primary
• Medicare Secondary Workers’ Compensation
• Medicare Secondary Public Health Service (PHS) or another Federal Agency
• Medicare Secondary Black Lung
• Medicare Secondary Veteran’s Administration
• Medicare Secondary Disabled Beneficiary Under Age 65 with Large Group Health Plan
• Medicare Secondary other liability insurance is primary
• Workers’ Compensation Medicare Set-aside Arrangement
• Effective Date – the date that indicates the start of the primary insurer's coverage.
• Termination Date – the date that indicates the termination of the primary insurer's coverage. No date in this field means the primary insurance coverage has not been terminated.
• Diagnosis Codes – only ICD codes are provided
• Policy Number – the primary insuring organization’s policy number for the Medicare beneficiary.
• Group Number – the group number of the insurance plan.
• Patient Relationship – the person subscribing to or carrying the insurance plan.
• Insurer Name – the name of the insurance company furnishing the coverage.
• Address – primary address of the insurer.
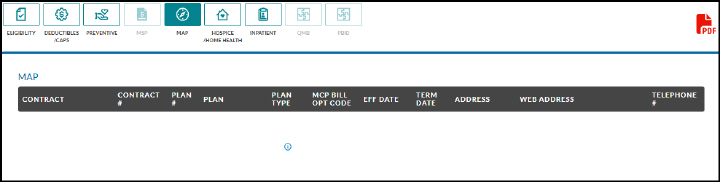
Medicare Advantage Plan (MAP) Figure 10: MAP Information
The
MAP tab displays data regarding the beneficiary’s enrollment, as applicable, in one or more of the following plans:
• Medicare Advantage (MA)
• Part D contracts
• MA Managed Care Plans (i.e., Part C contracts) that provide Part A and B benefits for beneficiaries enrolled under a contract.
The MAP page will include the following information (when applicable):
• Contract Number / Plan Benefit Package ID - the contract number followed by the plan number (if on file).
• Plan Name – a descriptive name of the beneficiary’s insurance coverage organization.
• Plan Type – a full plan description followed by Plan Type code, which may be any of the following types:
• Health Maintenance Organization Medicare Non Risk – HM
• Health Maintenance Organization Medicare Risk – HN
• Indemnity – IN
• Preferred Provider Organization – PR
• Point of Service – PS
• Pharmacy – Part D
• Effective Date – the date that indicates the start of enrollment in the coverage plan.
• Termination Date – the date that indicates the termination of enrollment to the coverage. No date in this field means the plan enrollment has not been terminated.
• MCO Bill Option Code (when applicable) – the bill option code of the Plan Type. This field only applies to plan types HM, HN, IN, PR, and PS (as defined above). This field will not be displayed for Part D plan type.
• Address/Phone Number – the contact information for the beneficiary’s insurance coverage organization.
• Contract website Address (when applicable) – the website address that will furnish information regarding the beneficiary’s insurance coverage.
The display and accessibility of information in Plan Coverage are contingent upon the availability of active data. It is the responsibility of the insurer to notify the Social Security Administration (SSA) of the plan and of any information associated with the plan (e.g., policy number, name of insurer). Once the SSA has been notified, the information will be shared with CMS’ systems, including its HETS.
Figure 11: Hospice/Home Health Information Results
The Hospice/Home Health page will include the following information (when applicable):
• Beneficiary’s Home Health Care information:
• HHEH Start Date – the date the 60-day home health episode period began.
• HHEH End Date – the date the 60-day home health episode period terminated.
• HHEH DOEBA Date – the date of earliest billing activity for spell of illness.
• HHEH DOLBA Date – the date of latest billing activity for spell of illness.
• Patient Status Code
• Patient Status Code
• Notice of Admission Indicator
• Provider number
• Contractor Name
• Contractor Number
• Home Health Certification
• Home Health Recertification
• Hospice information:
• Effective Date
• Termination Date
• Provider number
• Revocation Code
Figure 12: Inpatient Information Results
The Inpatient page will include the following information:
• Hospital Information
• Full Days Remaining ($0 per day)
• Co-payment Days Remaining
• Co-payment Amount per Day
• Lifetime Reserve Days
• Hospital Stay
• DOEBA date – the date of the earliest billing activity for the spell of illness.
• DOLBA date – the date of the latest billing activity for the spell of illness.
• Hospital stay start date
• Hospital stay end date
• Billing NPI
• Skilled Nursing Facility (SNF) information:
• DOEBA date
• DOLBA date
• SNF Days Full Days Remaining
• SNF Co-payment Days Remaining
• Co-payment Amount per Day
• SNF Stay
• Start Date
• End Date
• Billing NPI
• Psychiatric Information
• Lifetime Psychiatric Base Days
• Lifetime Psychiatric Remaining Days
Qualified Medicare Beneficiary (QMB) Figure 13: QMB information results
The QMB page will include the following information:
• Medicaid enrollment
• Effective Date – The date that indicates the start of eligibility for QMB enrollment.
• Termination Date – The date that indicates termination of eligibility for QMB enrollment. If the response indicates the QMB enrollment has terminated, please verify the patient’s QMB status through the State online Medicaid eligibility systems or other documentation.
• Plan Type
• Part A Deductible
• Deductible Year – This field will display the deductible year.
• Deductible – This field will always display 0 for a Qualified Medicare Beneficiary.
• Remaining Deductible – This field will be blank for a Qualified Medicare Beneficiary.
• Part B Deductible
• Deductible Year – This field will display the deductible year.
• Deductible – This field will always display 0 for a Qualified Medicare Beneficiary.
• Remaining Deductible – This field will be blank for a Qualified Medicare Beneficiary.
• Coinsurance Percentage – This field will always display 0 for a Qualified Medicare Beneficiary.
• Inpatient Spell
• DOEBA Date – Earliest Billing Date
• DOLBA Date – Latest Billing Date
• Hospital Information
• Co-Payment Amount – This field will always display 0 for a Qualified Medicare Beneficiary.
• Co-Payment Days Remaining – The hospital inpatient co-payment days remaining.
• Full Days Remaining – The full hospital inpatient days remaining in the spell.
• Skilled Nursing Facility (SNF) information:
• Full Days Remaining – The full SNF inpatient days remaining in the spell.
• Co-payment Amount – The amount of the inpatient co-payment. This field will always display 0 for a Qualified Medicare Beneficiary.
• Co-payment days remaining – The SNF inpatient co-payment days remaining.
Part B Immunosuppressant Drug Benefit (PBID) The PBID benefit allows individuals with end stage renal disease (ESRD) who received a successful kidney transplant to continue receiving Medicare Part B coverage for immunosuppressive drugs without a time limit.
Figure 14: PBID information results
The PBID page will include the following Part B information:
• Effective Date - the date that indicates the start of eligibility for PBID benefit.
• Termination Date - the date that indicates termination of eligibility PBID benefit.
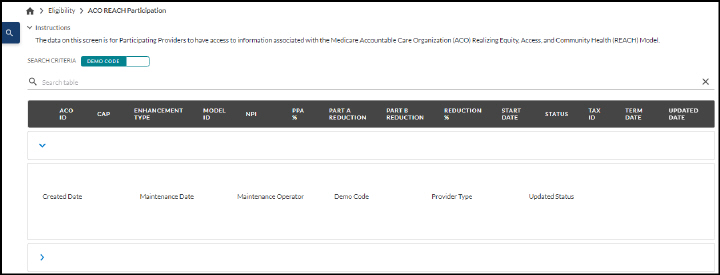
This feature provides participants and preferred providers in the Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) Model (previously named Global and Professional Direct Contracting (GPDC) Model access to their effective payment mechanisms or benefit enhancements.
To obtain ACO REACH information, select the Eligibility option on the SPOT toolbar and then select ACO REACH Participation from the dropdown menu.
Figure 15: Eligibility menu
Enter the Demo code and click Submit.
Figure 16: Part A ACO REACH Participation screen
Select the dropdown arrow in the front of a row to view the details.
Figure 17: Part A ACO REACH Participation details screen
No search fields are required. Click the magnifying glass in the blue box to select a Record Status (A or I), or enter an ACO Type and click Submit, if desired.
Figure 18: Part B ACO REACH Participation screen
Select the dropdown arrow in the front of a row to view the details.
Figure 19: Part B ACO REACH Participation details screen
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.