Last Modified: 5/30/2025
Location: FL, PR, USVI
Business: Part A
Q: We are receiving reject reason code 39929, so what steps can we take to avoid this reason code?
You can refer to
Part A reason code lookup for a description associated with the Medicare Part A reason code. Enter a valid reason code into the box and click the submit button.
A: You receive this reason code indicating the claim has rejected due to all line items rejecting or rejected and denied. There could be several reasons your claim is receiving this reject reason code; therefore, be sure to review each line item billed.
• If the claim is in a rejected status, you may adjust the claim, fix the line item, and resubmit.
Below are the most common line-item reason codes that reject with reason code 39929, based on First Coast's data.
• Here is the process for reviewing line-item rejects reason codes:
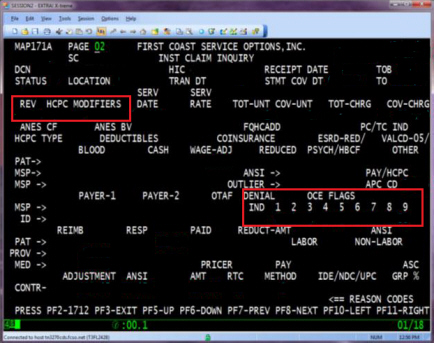
• Open the claim and go to page 02 (MAP171)
• Press the 'F2' key to review the line items details (MAP171D)
• Review each line-item reason code for all line items billed to determine what the error is
• Review the 201 report through DDE for history of the claims submitted.
31947 -- Non-covered charges are equal to the billed charges • Review the claim prior to submission to determine if the provider should be liable
• Condition code (CC) 20, 21 or occurrence code (OC) 32 is not present on the claim to indicate the non-covered reason
• CC 20 -- demand bills are submitted when the beneficiary is questioning coverage of a service and requests that the provider bill the claim to Medicare for review
• Submit only in cases when an advanced beneficiary notice (ABN) is not given or is not appropriate
• Submit all associated charges as non-covered
• Unrelated covered charges are allowed on the same claim
• Do not submit with OC 32
• CC 21 -- no-pay claims are submitted to obtain a denial from Medicare to facilitate payment by subsequent insurers (ex., statutory exclusions, outside original Medicare benefits, such as most self-administered drugs)
• Submit all associated charges as non-covered
• Modifier is not required to determine financial liability
• Medicare beneficiaries will always be liable for these claims
• Do not submit with OC 32
• OC 32 -- date(s) beneficiary notified of intent to bill (procedures or treatments), may not be reasonable or necessary under Medicare
• Provide the date(s) the ABN was signed by the beneficiary
• All services on the claim are associated with one particular ABN given on a specific date, unless the use of modifiers makes clear that not every line on the claim is linked to the ABN
• Submit additional dates when more than one ABN is tied to a single claim
• Line items using the GA modifier are considered related to the ABN and must be covered charges; other line items on the same claims may appear as covered or non-covered charges
• Do not submit with CC 20 or 21
C7251 -- Outpatient claim was billed, and the date of service is within the admission and discharge date of a skilled nursing facility (SNF) inpatient Part A claim (type of bill (TOB) 21x or 22x) and a therapy code is present • Physical therapy, speech-language pathology, and occupational therapy services are bundled into the SNF's global per diem payment for a resident's covered Part A stay, which are referred to as “Major Category V“ of SNF consolidated billing
• Providers who furnish such services to SNF residents must always look to the SNF (rather than to Part B) for payment
• The SNF is responsible for billing therapy on a 22x TOB, even when the services are furnished during a non-covered stay
• SNF residents that fall below a Medicare skilled level of care may be moved out of the SNF (discharged) or transferred to the SNF's certified distinct part unit (DPU) of the Medicare non-certified area
• The beneficiary is no longer subject to the SNF consolidated billing rule and therapy services may be billed directly, or if billed by a SNF the claim should be submitted on a 23x TOB
• If the entire facility qualifies as a Medicare-certified SNF, all Part B therapy services must continue to be billed by the SNF on a 22x TOB
U5390 -- Date of service is within a home health episode • Institutional provider's billing outpatient physical therapy, speech-language pathology, and occupational therapy services are subject to home health consolidated billing
• Always check beneficiary eligibility prior to submitting claims to Medicare
• Learn more about
SPOT and how to register
• If the dates of service are within the home health episode, contact the home health agency to set an arrangement for reimbursement
• SPOT
• The beneficiary's home health information is available via the SPOT.
• Select the Hospice/Home Health link from the Benefits/Eligibility submenu
• The beneficiary's information will automatically display
U539S -- Cardiac rehabilitation services exceeding 36 sessions • Effective for dates of service on or after January 1, 2010, procedure codes
93797 and 93798 (both professional and institutional claims) that exceed 36 sessions and support frequency of service require the procedure code to be billed with the
KX modifier • Services will deny when the KX modifier is not present on claim that exceed the 36 sessions
• Sessions are limited to a maximum of 2 one-hour sessions per day (up to 36 sessions, over a period of up to 36 weeks)
• Option for an additional 36 sessions over an extended period of time if approved by Medicare contractor
• Ensure the documentation supports the medical necessity beyond 36 sessions
• SPOT
• The number of technical and professional cardiac therapy sessions used for a patient is available via the SPOT.
• Select the Deductible/Caps link from the Benefits/Eligibility submenu
• The beneficiary's information will automatically display
W7047 -- Service not separately payable, line items rejection • Items and services that are considered an integral part of another service that is paid under outpatient prospective payment system (OPPS)
• No separate payment is made for packaged incidental services
• For example: routine supplies, anesthesia, recovery room use, and most drugs are considered part of surgical procedure. Items mentioned are packaged into the ambulatory payment classification (APC) payment for the surgical procedure
• Reference the status indicator which identifies if the HCPCS code is paid under OPPS before submission of claim(s)
• The full list of status indicators and their definitions is published in Addendum D1 of the OPPS/ASC proposed and final rules each year
• For example, OCE System Flag 1:
HCPCS with a status indicator 'N' are packaged incidental services and are not considered payable
• Refer to
Outpatient Code Editor 
(OCE) which edits a claim for accuracy of submitted data in determining if packaging is applicable
• DDE
• The process for reviewing the OCE flag status indicators for the desired HCPCS codes is outlined below:
• Open the claim and go to page 02 (MAP171)
• Press the 'F2' or 'F11' key to review the line items details (MAP171A)
• Review the OCE flag status indicators (IND) 1 field
W7049 -- Service on the same day as inpatient procedure, line items denial • Outpatient items and services submitted with an inpatient procedure are not payable under outpatient prospective payment system (OPPS)
• All other line items on the same day as the line with a C status indicator are denied (line-item denial/rejection flag = 1, APC return buffer)
• Reference the status indicator which identifies if the HCPCS code is paid under OPPS prior to claim submission
• The full list of status indicators and their definitions is published in Addendum D1 of the OPPS/ASC proposed and final rules each year
• For example, OCE System Flag 1:
HCPCS with a status indicator 'C' are inpatient procedures and are not considered payable
• Refer to
Outpatient Code Editor 
(OCE) which edits a claim for accuracy of submitted data in determining if packaging is applicable
• If the HCPCS code is incorrect, you may request a corrected claim to appeals
• DDE
• The process for reviewing the OCE flag status indicators for the desired HCPCS codes is outlined below:
• Open the claim and go to page 02 (MAP171)
• Press the 'F2' or 'F11' key to review the line items details (MAP171A)
• Review the OCE flag status indicators (IND) 1 field
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.








 (OCE) which edits a claim for accuracy of submitted data in determining if packaging is applicable
(OCE) which edits a claim for accuracy of submitted data in determining if packaging is applicable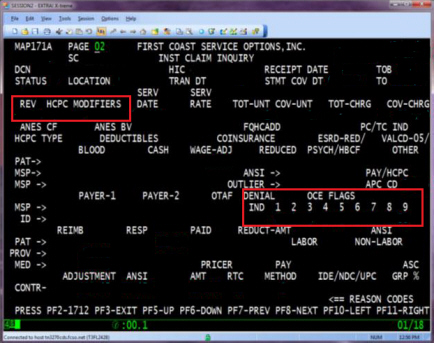

 (OCE) which edits a claim for accuracy of submitted data in determining if packaging is applicable
(OCE) which edits a claim for accuracy of submitted data in determining if packaging is applicable