Home ►
Claim Reopening Gateway - Help Guide
Last Modified: 4/20/2024
Location: FL, PR, USVI
Business: Part B
Welcome to the First Coast Claim Reopening Gateway Help Guide. The Claim Reopening Gateway is an interactive tool that requires no registration or enrollment, and offers a quick and easy way to make Part B claim corrections directly on the First Coast website. Though the tool is designed to mirror the claim reopening process in First Coast’s Secure Provider Online Tool (SPOT), this gateway can be used by any provider, whether they are enrolled in SPOT or not. The only requirement needed to use the gateway is to have internet access and to validate the provider using the National Provider Identifier (NPI); Provider Transaction Access Number (PTAN); and the last five digits of the Tax Identification Number (TIN).
Note: Please have your remittance advice available to refer to claim details while using the gateway.
While on the First Coast website, hover over the Tools Center option near the bottom of the left navigation menu, then go to Appeals, and Reopening Gateway.
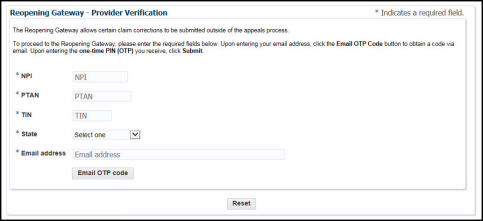
Once you have navigated to the gateway, click the “Accept” button on the disclaimer screen. Then you will see the provider verification page:
1. Enter your NPI, PTAN, and the last five digits of your TIN. Then, select your state, enter a valid email address, and click the “Email OTP code” button. You will quickly receive an email with the subject line “URGENT: Reopening Gateway access” that contains your code.
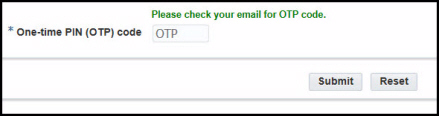
2. Enter your code in the One-time PIN (OTP) code box that appears after clicking “Email OTP Code.” Then, click “Submit.”
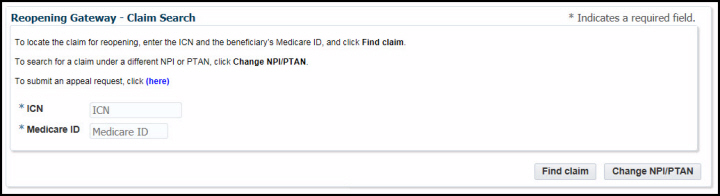
3. Next, the claim search screen will appear. Enter the claim’s internal claim number (ICN) and the beneficiary’s Medicare ID.
Click “Find claim” and the gateway will automatically determine if any line items are eligible for a reopening. You may also return to the previous screen if you need to look for a claim under a different provider by clicking the “Change NPI/PTAN” button.
NOTE: If the claim is
not eligible for a reopening, an error message will appear, and you may click “Appeal request” to be taken to the
appeals forms page on the website. View more information about the
restricted modifiers and procedure codes that apply to this gateway, which are the same for SPOT submissions. In addition, if the claim has been returned as unprocessable, has already been adjusted, or has been filed as unassigned, it is not eligible to be reopened via the gateway.
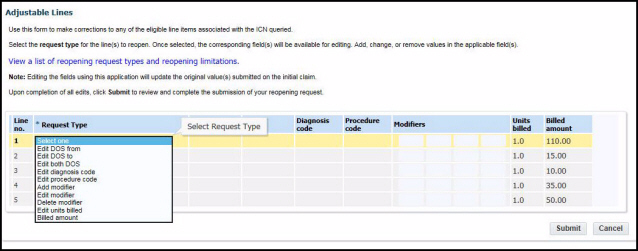
4. Once the gateway has determined that your claim is eligible for a reopening, the assigned eligible lines of the claim will appear. On the line you wish to correct, select your request type from the Request Type drop-down menu and enter the data you wish to change on your claim. Then click “Submit”:
The available request types are:
• Edit DOS from
• Edit DOS to
• Edit both DOS
• Edit diagnosis code
• Edit procedure code
• Add modifier
• Edit modifier
• Delete modifier
• Edit units billed
• Billed amount
Additional request types:
• Billed in error
• Report an entire claim or individual lines of a claim as billed in error. The claim must be fully or partially paid and have no Medicare Secondary Payer information in order to use this feature.
• History correction
• This option allows you to resubmit a claim without making any corrections. This option is only valid for the following scenarios:
• The beneficiary’s record has been corrected to indicate Medicare is now primary for the date(s) of service of the denied claim.
• The beneficiary’s record has been corrected to indicate the beneficiary is entitled to Medicare Part B for the date(s) of service of the denied claim.
• The beneficiary’s record has been corrected to indicate the beneficiary’s hospice election period no longer conflicts with the date(s) of service of the denied claim.
• The beneficiary’s record has been corrected to indicate the beneficiary is no longer covered by a Medicare Advantage Plan for the date(s) of service on the denied claim.
• Medically Unlikely Edits (MUE) denials involving two claims that were submitted at the same time; resulting in a MUE denial along with a duplicate claim denial.
NOTE: View further instructions, comments, and limitations for request types
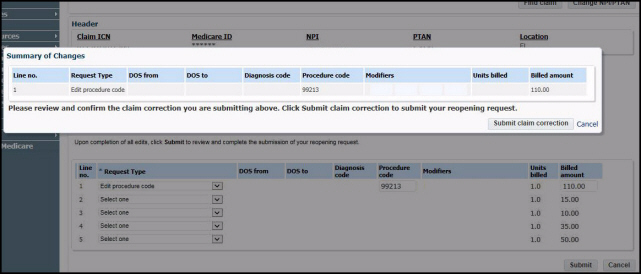
here. 5. After clicking “Submit,” a summary of changes screen will appear. Review them for accuracy, and if they are acceptable, click the “Submit claim correction” button. If they are not accurate, click “Cancel” and you will be returned to the adjustable lines page to make any necessary corrections. Once you have made your corrections, click “Submit” again and review the summary of changes. If the changes are acceptable, click “Submit claim correction.”
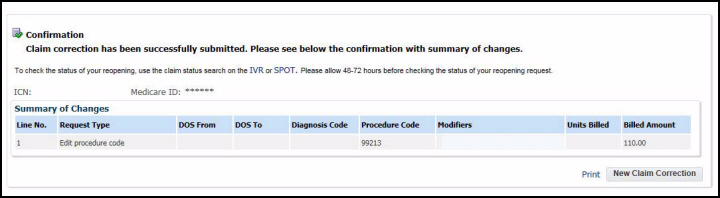
6. A confirmation screen will appear. You can click “Print” or “New Claim Correction”:
7. If you have more claims to reopen, click the “New Claim Correction” button and the gateway will return you to the claims search page, where you can enter the next ICN and Medicare ID. If the claims are not for the same provider, click the “Change NPI/PTAN” button to return to the provider verification page to enter the new provider information.
NOTE: You may check the status of your reopening using the interactive voice response (IVR) or SPOT. Please allow 48-72 hours before checking the status.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.