Last Modified: 4/6/2024
Location: FL, USVI, PR
Business: Part A
A same day transfer occurs if the beneficiary is admitted to your facility and is expected to stay overnight, but transfers to a different facility.
Same day transfer to participating hospital:
• Patient must be admitted with the expectation they will remain overnight
• Transferring hospital paid based on per diem rate
• The day is counted for cost report and pricer purposes for both facilities
• Utilization days are charged to the patient's benefit period per the receiving facility
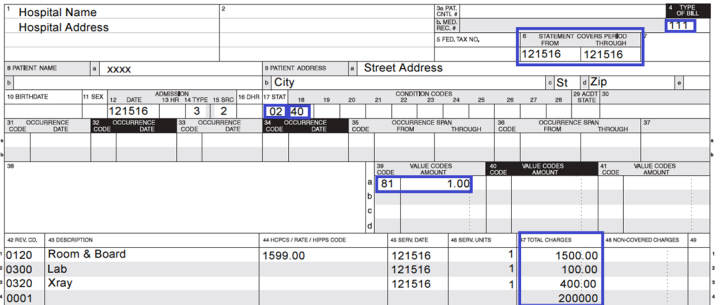
Billing instructions for transferring hospital:
• Condition code 40
• Same “From” and “Through” dates
• Admit date is the same as the "From" and "Through" dates
• Appropriate patient status code
• One non-covered day
• Charges and units are covered
Patient left against medical advice:
• Patient status code 07
• Patient is readmitted to another facility the same day
• Original discharging hospital must code their claim as a discharge to the subsequent facility
• Submit adjustment if claim is already submitted
• Transfer payment policy applies
A SNF same day transfer is when the patient admits to a SNF and is expected to remain overnight but was transferred to another participating provider (acute care hospital or another SNF) before the following midnight.
Billing instructions for transferring SNF:
• One non-covered day
• Default Health Insurance Prospective Payment System (HIPPS) code ZZZZZ allowed
• Condition code 40
• Appropriate patient status code
• Charges submitted as covered
• Admission date, statement “From” and “Through” dates are same
Ancillary charges:
• If the patient returns to and is readmitted to the same acute care PPS hospital, they just left for symptoms related the prior stay's medical condition, the SNF bills the hospital for ancillary services which occurred while in the SNF.
• If the patient returns to the hospital for reasons unrelated to the previous admission or transfers to a different hospital or facility, then the SNF may bill Medicare for ancillary charges. The day does not count as a Medicare utilization day unless the patient transfers to a nonparticipating facility.
Common Errors
1. A claim is billed with patient discharge status codes 01 (patient discharged to home or self-care); however the beneficiary was transferred to another facility. An adjustment needs to be submitted to correct patient status code.
2. A claim is billed with patient discharge status codes 01 (patient discharged to home or self-care). After the patient went home, they later went to another hospital on same day and were admitted. An adjustment needs to be submitted to correct patient status code to 02 (discharged/transferred to a short-term general hospital for inpatient care).
References:
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.