Last Modified: 4/1/2024
Location: FL, USVI, PR
Business: Part A
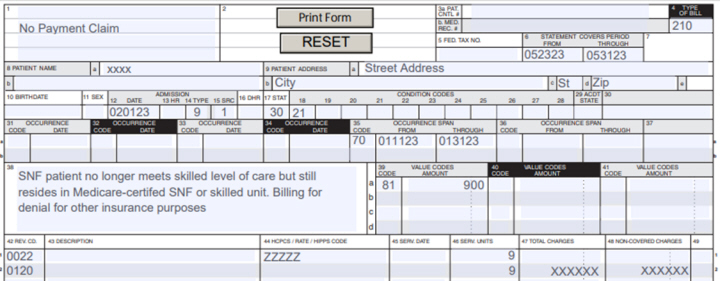
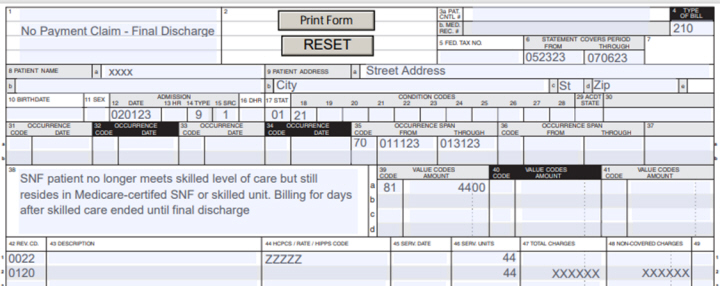
Providers must submit no-payment bills for beneficiaries that previously dropped to non-skilled care but continue to reside in the Medicare-certified area of the facility. No-payment billing starts the day following the date that active care ended.
Providers may submit these claims using the default health insurance prospective payment system (HIPPS) code ZZZZZ in addition to an appropriate room and board revenue code only. No further ancillary services need reported on these claims.
There are two types of no payment claims:
• Patient previously dropped to non-skilled level of care - denial needed for other insurer
• Patient previously dropped to non-skilled level of care - final discharge
No-pay claims should continue to be bill until discharge or no longer in a Medicare-certified bed.
• Type of bill (TOB) 210 (SNF) or 180 for swing-beds (SB)
• Statement covers from and through dates
Begins the day after the date active care ended
• Days and charges are non-covered beginning the date after active care ended
• Condition code 21 (billing for denial)
• OSC 70 with qualifying hospital stay dates
• Default HIPPS code ZZZZZ
• Patient status code (30 if still patient)
• Remarks to indicate lower level of care; need denial for other insurance purposes
In these cases, you must only submit the final discharge bill that may span multiple months but must be as often as necessary to meet timely filing guidelines. The claim may span both the provider and Medicare fiscal year end dates.
• TOB 210 (SNF) or 180 (SB)
• Statement covers from and through dates
Begins the day after the date active care ended
• Days and charges are non-covered beginning the date after active care ended
• Condition code 21 (billing for denial)
• OSC 70 with qualifying hospital stay dates
• Default HIPPS code ZZZZZ
• Patient status code other than 30 (still patient)
• Remarks to indicate lower level of care; billing for days after skilled care ended until final discharge
Consolidated billing (CB) requires you to furnish and bill for physical therapy, occupational therapy, and speech language pathology services when providing therapy during a non-covered stay in which the beneficiary, who is not eligible for Part A extended care benefit, still resides in a Medicare-certified SNF or distinct skilled unit.
SNF CB edits require you to bill for these services on TOB 22x (inpatient part B).
Unlike with benefits exhaust claims, Part B TOB 22x may be submitted prior to the submission of no payment claims, TOB 210.
When a change in level of care occurs after benefits exhaust, the SNF must submit the benefits exhaust bill in the next billing cycle indicating that active care has ended for the beneficiary.
If your facility has a separate distinct non-skilled area or wing, you may discharge those patients to this area using the appropriate patient discharge status code. No-payment bills would not be required. In addition, consolidated billing for therapy services would not apply for these patients.
No-payment bills are not required for non-skilled beneficiary admissions. They are only required for beneficiaries that have previously received covered care and subsequently dropped to non-covered care but continue to reside in the certified area of the facility.
References
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.