Last Modified: 6/10/2022
Location: FL, PR, USVI
Business: Part A
Section 1833(t)(1)(B)(i) of the Act allows the CMS to define the services for which payment under the outpatient prospective payment system (OPPS) is appropriate. Services designated as “inpatient only” are not appropriate to be furnished in a hospital outpatient department.
Generally, but not always, "inpatient-only” services are surgical services that require inpatient care because of the:
• Nature of the procedure,
• Typical underlying physical condition of patients who require the service, or
• Need for at least 24 hours of postoperative recovery time or monitoring before the patient can be safely discharged.
No payment is made for an “inpatient-only” procedure submitted on the outpatient hospital type of bill, 13X. No payment is made for other services rendered on the same day as the “inpatient-only” procedure.
An example of an “inpatient-only” service is CPT code 33513, “Coronary artery bypass, vein only; four coronary venous grafts.”
The designation of services to be “inpatient-only” is open to public comment each year as part of the annual rulemaking process.
Procedures removed from the “inpatient-only” list may be furnished in either the inpatient or outpatient setting and continue to be payable when furnished in the inpatient setting.
There is no payment under OPPS for services that CMS designates to be “inpatient-only” services.
Instructions
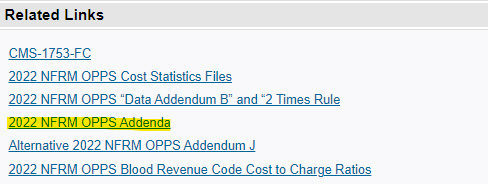
After clicking on the above link to hospital outpatient regulations and notices, click on the regulation number for the appropriate final rulemaking year requested (CMS-xxxx-FC).
Then:
Click on the “20XX NFRM OPPS Addenda” listed under related links.
Next:
Click "Accept" on the License Agreement page. Once you click "Accept" a dialog box will appear asking you to "save" or "open."
Finally:
Once you open, you will get a box with a list of the addenda available. Choose addendum E (.xlsx or .csv); double click to open the file, then search for the code in question (CTRL F to open search box).
There are two exceptions to the policy of not paying for outpatient services rendered on the same day as an “inpatient-only” service paid under OPPS if the inpatient service had not been furnished.
Exception 1
“Inpatient-only” service defined in CPT as a “separate procedure”, and other services billed with the “inpatient-only” service that can be paid under OPPS:
• OPPS SI = T on the same date as the “inpatient-only” procedure, or
• OPPS SI = J1 on the same claim as the “inpatient-only” procedure
The “inpatient-only” service is denied, but payment is made for the separate procedure and any remaining payable OPPS services.
Exception 2
“Inpatient-only” service is furnished, but the patient dies before inpatient admission or transfer to another hospital.
The hospital reports the “inpatient-only” service with modifier “CA” (Procedure payable only in the inpatient setting when performed emergently on an outpatient who expires prior to admission).
A single payment is made for all services reported on the claim, including the “inpatient-only” procedure.
Hospitals should report modifier CA on only one procedure.
If an "inpatient-only" procedure is performed in the outpatient setting, and the patient is subsequently admitted as an inpatient, the "inpatient-only” procedure can be reported on the inpatient claim when the services are:
• Provided on the date of inpatient admission.
• Provided within three days of inpatient admission.
• Deemed related to inpatient admission per the payment window policy.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.



 webpage.
webpage. 
 documentation.
documentation.