Home ►
EM ►
E/M interactive worksheet: Help guide
Last Modified: 7/3/2024
Location: FL, PR, USVI
Business: Part A, Part B
Evaluation and management (E/M) services refer to visits furnished by physicians and qualified, licensed, non-physician practitioners. Billing Medicare for a patient visit requires the selection of the code that best represents the level of E/M service performed.
The purpose of this interactive worksheet is to assist providers with identifying the appropriate E/M code based upon either the:
• 1995 or 1997 Documentation Guidelines for Evaluation and Management Services, or
• AMA CPT E/M Code Guideline Changes for 2021 (effective for office and outpatient visits for dates of service on and after January 1, 2021), or
• E/M Code and Guideline Changes for 2023 (effective for other E/M visits for dates of service on and after January 1, 2023).
Effective January 1, 2023, the AMA CPT Editorial Panel approved revised coding and updated guidelines for "Other E/M visits" (which includes hospital inpatient, hospital observation, emergency department, nursing facility, home or residence services, and cognitive impairment assessments). CMS adopted most of the CPT’s revised guidance, including deletion of several CPT codes.
Effective for dates of service (DOS) on and after January 1, 2023, practitioners have the choice to document most E/M visits via medical decision making (MDM) or time, except emergency department visits and cognitive impairment assessments, which are not timed services.
The E/M code and guideline changes are like those already applied to office and other outpatient visits, which were effective for dates of service on and after January 1, 2021.
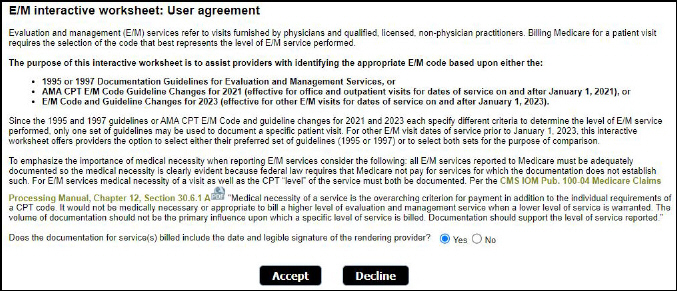
CMS requires that any Medicare service provided or ordered must be authenticated by the author -- the one who provided or ordered that service. Before completion of the E/M worksheet is initiated, verification that this requirement has been fulfilled is completed. Next, before beginning an
E/M interactive worksheet session, you must first accept the terms of the E/M interactive worksheet, the user agreement. Although the E/M interactive worksheet was created as a resource to assist providers with selecting the appropriate E/M code, it is not intended to serve as a replacement for the E/M documentation guidelines published by CMS, AMA CPT E/M Code Guideline Changes for 2021 (effective for office/outpatient visits only for dates of service on and after January 1, 2021), or AMA CPT Code and Guideline changes for 2023 (effective for other services on and after January 1, 2023.
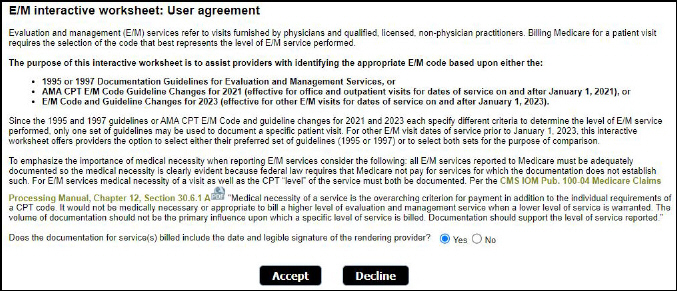
Note: Once you have responded that documentation for services billed includes the date and legible signature of the rendering provider, you will be asked to acknowledge and accept the terms of the user agreement. Once accepted, you will gain immediate access to the E/M interactive worksheet.
Since the E/M worksheet is designed to be interactive, your selections will directly affect the calculation of the suggested E/M code. Therefore, before beginning your E/M interactive worksheet session, it is strongly recommended that you have the following available:
• Patient’s medical record
• Current Procedural Terminology (CPT) manual
Note: Several of these resources and additional supporting information can be found by clicking on the Helpful Resources informational icon at the top of the worksheet.
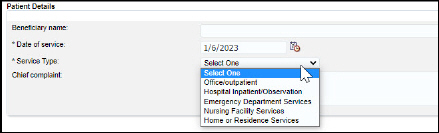
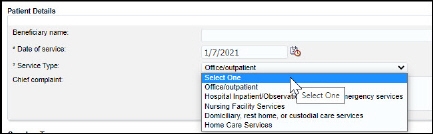
Next, there is a requirement to specify the details of the encounter. Using the patient’s medical record as a reference, enter the following information:
• Beneficiary name
• Date of service (required)
• Service type (required)
• Chief complaint (CC) or purpose of the patient’s visit
The E/M
worksheet is designed to function based on the date of service and type of visit.
If the date of service is on or after January 1, 2023, the worksheet options are based on the AMA 2023 E/M code and guideline changes for 2023.
If the date of service is on / after 1/1/23, select from the following service types:
• Office / outpatient
• Hospital Inpatient / Observation
• Emergency Department Services
• Nursing Facility Services
• Home or Residence
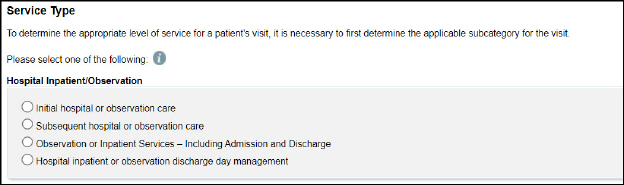
Once the service type is selected, corresponding subcategories will display. Select the subcategory applicable to the E/M services provided.
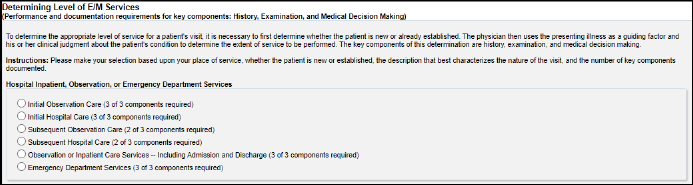
Here is an example of the subcategory options for Hospital Inpatient/Observation services:
Components for E/M code determination
Depending on the service type and subcategory selected, the E/M code may be determined via time and / or Medical Decision Making (MDM).
Use the presenting illness as a guiding factor and clinical judgment about the patient's condition to determine the extent of service to be performed. The key components of this determination are the medical decision making or total time E/M services are performed.
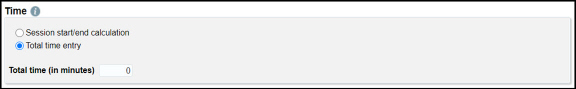
Time may be documented or recorded as multiple entries that will be aggregated for that date of service or in a free-form manner combining all with a single entry.
Based on information submitted, the worksheet will provide an aggregated summation and corresponding code.
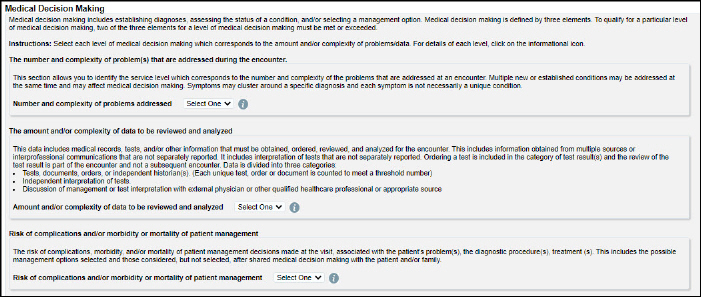
Medical decision making includes establishing diagnoses, assessing the status of a condition, and/or selecting a management option. To qualify for a particular level of medical decision making, two of the three elements for a level of medical decision making must be met or exceeded.
Selections for each element are made, with a level of medical decision making determined by the worksheet, and a corresponding, suggested code displayed. To assist with selections, view details for each level by clicking on the informational icons. In addition, the Helpful Resources icon provides links to resources including the
AMA CPT E/M changes for 2023.

If the date of service is prior to 1/1/23 select from the following service types:
• Office / outpatient
• Hospital Inpatient / Observation, including Emergency Services
• Nursing Facility Services
• Domiciliary, rest home, or custodial care services
• Home Care Services
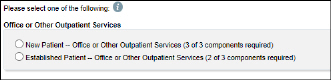
Once the service type is selected, corresponding subcategories will display. Select the subcategory applicable to the E/M services provided.
Here is an example of the subcategory options for Office / outpatient services:
Select whether the patient is new or already established.
The components for E/M code determination for office / outpatient services will be similar to the options displayed above for 2023 codes. Informational icons will provide support along with the helpful resources icon which provides a link to the AMA guidance for office / outpatient visits on / after 1/1/21.
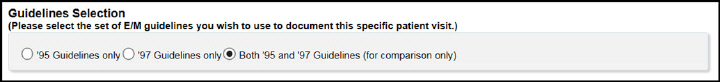
When non-office/outpatient related services are selected for dates of service prior to January 1, 2023, the worksheet is based upon the performance and documentation requirements within the 1995 and 1997 Documentation Guidelines for Evaluation and Management Services.
Since the 1995 and 1997 guidelines each specify different criteria to determine the level of E/M service performed, only one set of guidelines may be used to document a specific patient visit. The E/M interactive worksheet offers providers the option to select either one set of guidelines (1995 or 1997) or both for the purpose of comparison.
Note: The primary difference between the 1995 and 1997 E/M documentation guidelines pertains to the requirements to qualify for specific Examination levels. Each set of guidelines specifies different requirements regarding possible examination types as well as criteria for each examination level. These differences will be outlined in the Examination section of this guide.
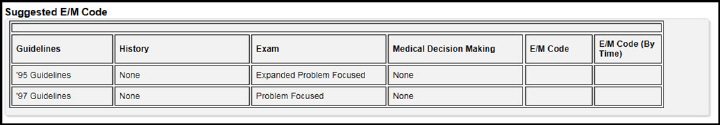
Options available:
• Both ’95 and ’97 Guidelines (default) -- if this option is selected, the E/M interactive worksheet will display History and Examination choices, E/M Tooltips, and requirements pertaining to both sets of E/M documentation guidelines.
Note: If this option is selected, all sections of the E/M interactive worksheet -- including both the 1995 and 1997 Examination sections -- must be completed in order for the worksheet to calculate the suggested E/M code correctly. In addition, the At least 4 Associated Comorbidities option and the At least 3 Chronic/Inactive Conditions option in the HPI subsection will both be displayed.
• ’95 Guidelines only -- if this option is selected, the E/M interactive worksheet will display only History and Examination choices, E/M Tooltips, and requirements pertaining to the 1995 Documentation Guidelines for Evaluation & Management Services. The calculation of the suggested E/M code will be based exclusively on the user’s selections and the 1995 guidelines.
Note: If this option is selected, the 1997 Examination section and all associated 1997 E/M Tooltips will not be displayed.
• ’97 Guidelines only -- if this option is selected, the E/M interactive worksheet will display only History and Examination choices, E/M Tooltips, and requirements pertaining to the 1997 Documentation Guidelines for Evaluation and Management Services. The calculation of the suggested E/M code will be based exclusively on the user’s selections and the 1997 guidelines.
Note: If this option is selected, the 1995 Examination section and all associated 1995 E/M Tooltips will not be displayed.
Tip: Although the default option is Both ’95 and ’97 Guidelines, it is recommended that only one set of guidelines (1995 or 1997) is selected to avoid confusion.
To determine the appropriate level of service for a patient's visit, it is necessary to first determine whether the patient is new or already established. The physician then uses the presenting illness as a guiding factor and his or her clinical judgment about the patient's condition to determine the extent of service to be performed. The key components of this determination are History, Examination, and Medical Decision Making.
Here is an example of the E/M services section for Hospital Inpatient, Observation, or Emergency Department Services
The Determining Level of E/M Services section defines the category of patient visit and not only determines how many of the key components must be performed and documented but also the specific requirements, as specified in both the 1995 and 1997 documentation guidelines, for the PFSH element of the History component.
In the Determining Level of E/M Services section, your selection should be based upon the following information (as indicated within the patient’s medical record):
• Place of service (e.g., office, outpatient, hospital, nursing facility, rest home, home)
• Type of patient (e.g., new, established) or nature of the visit (e.g., initial, subsequent, inpatient, observation)
• Number of key components performed and documented (e.g., History, Examination, and Medical Decision Making)
Note: Since the 1995 and 1997 E/M documentation guidelines specify different PFSH requirements based on the category of patient visit, the Determining Level of E/M Services section should be completed before making selections within the History section.
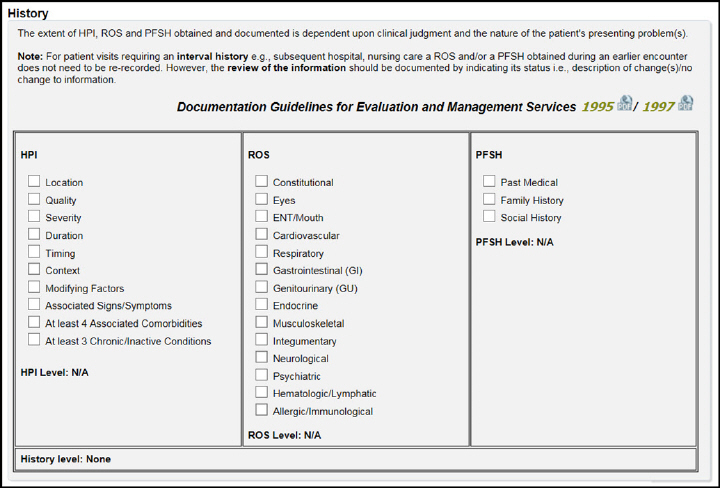
The History section is comprised of three subsections:
• History of present illness (HPI) -- a chronological description of the development of the patient’s present illness from the first sign and/or symptom or from the previous encounter to the present.
• Review of systems (ROS) -- an inventory of body systems obtained by asking a series of questions in order to identify signs and/or symptoms that the patient may be experiencing or has experienced.
• Past medical history, family history, social history (PFSH) -- a review of the patient’s past medical history (e.g., previous illnesses, injuries, operations), family history (e.g., potential hereditary conditions), and an age-appropriate review of patient’s social history (current and past activities).
The total History level will be automatically calculated by the E/M interactive worksheet based upon choices made in each subsection (e.g., HPI, ROS, and PFSH), the Guidelines Selection section, and the Determining Level of E/M Services section.
The 1995 and 1997 E/M documentation guidelines specify the following requirements to determine the total level of History: 3 out of 3 elements must be met or exceeded.
HPI |
ROS |
PFSH |
History Level |
Brief |
N/A |
N/A |
Problem Focused |
Brief |
Problem Pertinent |
N/A |
Expanded Problem Focused |
Extended |
Extended |
Pertinent |
Detailed |
Extended |
Complete |
Complete |
Comprehensive |
Note: Levels for three out of three History elements (i.e., HPI, ROS, and PFSH) must meet or exceed the requirements specified for each level of History (i.e., Problem Focused, Expanded Problem Focused, Detailed, or Comprehensive).
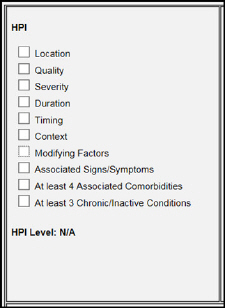
There are two possible levels of HPI:
• Brief -- 1995 and 1997 E/M documentation guidelines -- at least one to three elements of the present illness must be documented in the medical record.
• Extended -- either four or more elements of the present illness or four or more associated comorbidities or the status of three or more associated chronic or inactive conditions must be documented in the medical record.
Your selections in the HPI subsection should be based on the documentation contained within the patient’s medical record that describes the details surrounding the chronological development of the present illness, from the first sign or symptom of the illness to its status at the time of the visit being documented. While making your selections, use your cursor to reveal E/M Tooltips that will help you identify the quantifying elements of the HPI.
The HPI level will be automatically calculated by the E/M interactive worksheet based upon the entries within this subsection as well as the guidelines selected (1995, 1997, or both).
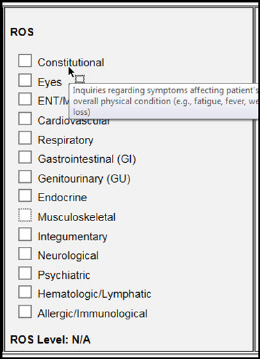
The options available within the ROS subsection of the E/M interactive worksheet are identical regardless of the guidelines selected. There are four possible levels of ROS:
• N/A -- no inquiries regarding the system directly related to the symptom(s) identified in the HPI or any other system are documented in the medical record.
• Problem Pertinent -- inquiries regarding the system directly related to the symptom(s) identified in the HPI are documented in the medical record.
• Extended -- inquiries regarding the system directly related to the symptom(s) identified in the HPI and between two and nine additional systems are documented in the medical record.
• Complete -- inquiries regarding the system directly related to the symptom(s) identified in the HPI and all additional systems are documented in the medical record.
Note: A total of at least ten organ systems should be reviewed and documented.
Your selections in the ROS subsection should be based on those details contained within the patient’s medical record that describe the series of questions asked by the physician (along the with the patient’s pertinent positive and negative responses) that help identify signs and/or symptoms the patient has experienced and provide an inventory of affected systems. While making your selections, use your cursor to reveal E/M Tooltips that will help you identify the systems reviewed and documented within the patient’s medical record.
The ROS level will be automatically calculated by the E/M interactive worksheet based upon the entries within this subsection.
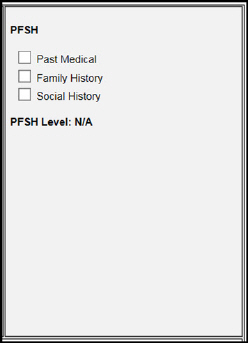
Although PFSH is one of the easiest elements of History to document, determining the appropriate level of PFSH can cause some confusion even among experienced coders. The primary reason for the confusion is that although both the 1995 and 1997 E/M documentation guidelines specify the same requirements to determine the level of PFSH, the requirements for each level differ based upon the category of visit being documented.
There are three possible levels of PFSH:
• N/A -- no inquiry or review of any of the three PFSH areas is documented in the medical record.
• Pertinent -- a review of at least one specific item from any of the three PFSH areas directly related to the problem(s) identified in the HPI is documented in the medical record.
• Complete -- a review of two or all three of the PFSH areas -- depending upon the category of E/M service -- is documented in the medical record.
The 1995 and 1997 guidelines both specify the following: A review of all three history areas is required for services that by their nature include a comprehensive assessment or reassessment of the patient. The E/M documentation guidelines also specify which categories of visits require comprehensive assessments as well as three out of three PFSH elements to be documented within the medical record to attain a Complete level of PFSH:
• New Patient -- Office or Other Outpatient Services
• Initial Observation Care
• Initial Hospital Care
• Observation or Inpatient Care Services -- Including Admission and Discharge
• Initial Nursing Facility Care
• Annual Nursing Facility Assessment
• New Patient -- Domiciliary, Rest Home, or Custodial Care Services
• New Patient -- Home Care Services
Your selections in the PFSH subsection should be based on those details contained within the patient’s medical record that describe the physician’s review of the patient’s past medical history (e.g., previous illnesses, injuries, operations), family history (e.g., potential hereditary conditions), and an age-appropriate review of patient’s social history (current and past activities). While making your selections, use your cursor to reveal E/M Tooltips that will help you identify the quantifying elements of the PFSH.
The E/M interactive worksheet will automatically calculate the appropriate level of PFSH based upon the user’s selection in the Determining Level of E/M Services section as well as the number of options selected in the PFSH subsection.
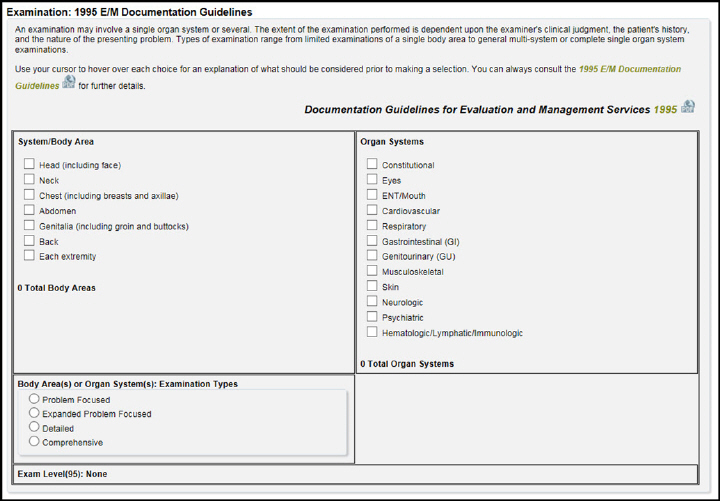
There are two examination sections incorporated into the E/M interactive worksheet:
• Examination: 1995 E/M Documentation Guidelines
• Examination: 1997 E/M Documentation Guidelines
Since each is based upon the specific guidelines referenced, the user’s selection in the Guidelines Selection section will determine which examination sections will be visible during a particular E/M session. If the option Both '95 and '97 Guidelines is selected, both examination sections must be completed for the E/M interactive worksheet to automatically calculate a suggested E/M code.
This examination section will only be visible if either ’95 Guidelines only or Both '95 and '97 Guidelines is selected. An examination based on the 1995 E/M documentation guidelines may involve a single organ system or several. The extent of the examination performed is dependent upon the examiner’s clinical judgment, the patient’s history, and the nature of the presenting problem. Types of examination range from limited examinations of a single body area to general multi-system or complete single organ system examinations.
Your selections in the Body Areas and Organ Systems subsections should be based on those details contained within the patient’s medical record that describe the physician’s examination of the patient. While making your selections, use your cursor to reveal E/M Tooltips that will help you identify the quantifying elements of each body area or system in accordance with 1995 E/M documentation guidelines.
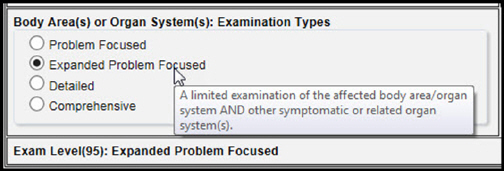
However, since the quality or extent of the physician’s examination is subjective and based upon clinical judgment, the E/M interactive worksheet cannot calculate the 1995 Examination level automatically. The 1995 Examination level is determined by your selection in the Body Area(s) or Organ System(s): Examination Types subsection. However, E/M Tooltips, based on 1995 guidelines, will assist you with determining the appropriate 1995 Examination level:
Note: Once you have made your selection in the Body Area(s) or Organ System(s): Examination Types subsection, the E/M interactive worksheet will use the specified 1995 Examination level in its final calculation of the suggested E/M code based upon 1995 E/M documentation guidelines.
Examination Levels |
Body Area(s) or Organ Systems: ‘95 Guidelines |
Problem Focused |
A limited examination of the affected body area or organ system. |
Expanded Problem Focused |
A limited examination of the affected body area/organ system
AND other symptomatic or related organ system(s). |
Detailed |
An extended examination of the affected body area(s)
AND other symptomatic or related organ systems. |
Comprehensive |
A general multi-system examination (including 8 or more organ systems) OR a complete examination of a single organ system |
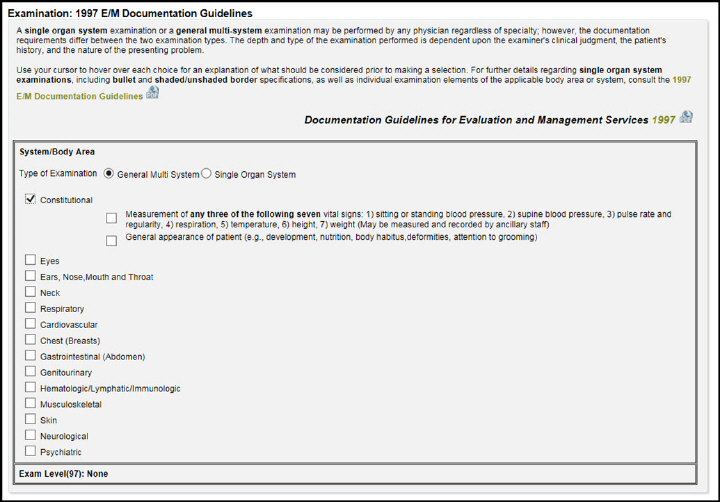
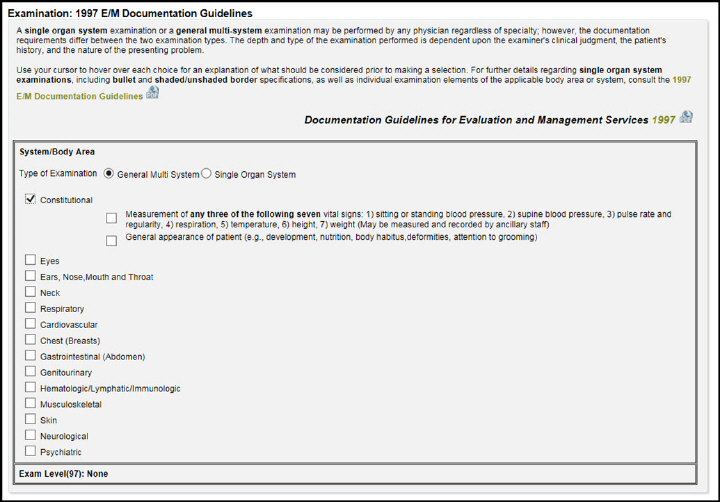
This examination section will only be visible if either ’97 Guidelines only or Both '95 and '97 Guidelines is selected. According to the 1997 E/M documentation guidelines, a single organ system examination or a general multi-system examination may be performed by any physician regardless of specialty; however, the documentation requirements differ between the two examination types. The depth and type of the examination performed is dependent upon the examiner’s clinical judgment, the patient’s history, and the nature of the presenting problem.
Your selections in the General Multi System and Single Organ System subsections should be based on those details contained within the patient’s medical record that describe the physician’s examination of the patient. While making your selections, use your cursor to reveal E/M Tooltips that are based on general multi-system examination requirements.
Note: Please refer to the tables contained within the 1997 E/M Documentation Guidelines for specific content criteria for single organ system examinations -- including bullet and shaded/unshaded border specifications -- as well as individual examination elements of the applicable body area or system.
The 1997 Examination level is automatically determined by your selection in either the Single Organ System: Examination Types subsection or the General Multi-System: Examination Types subsection.
Once you have made your selection in either the Single Organ System: Examination Types subsection or the General Multi-System: Examination Types subsection, the E/M interactive worksheet will use the specified 1997 Examination level in its final calculation of the suggested E/M code based upon 1997 E/M documentation guidelines.
Examination Levels |
Single Organ System -- ‘97 Guidelines |
General Multi-System -- ‘97 Guidelines |
Problem Focused |
Examination should include performance and documentation of 1-5 bulleted elements. |
Examination should include performance and documentation of 1-5 bulleted elements for one or more organ systems or body areas. |
Expanded Problem Focused |
Examination should include performance and documentation of at least 6 bulleted elements. |
Examination should include performance and documentation of at least 6 bulleted elements for one or more organ systems or body areas. |
Detailed |
Examination should include performance and documentation of at least 12 bulleted elements. Exception: Eye and psychiatric examinations require only 9 bulleted elements |
Examination should include performance and documentation of at least 2 bulleted elements for at least six organ systems or body areas
OR
At least 12 bulleted elements for two or more organ systems/body areas. |
Comprehensive |
Examination should include performance of ALL bulleted elements. Note: Documentation of ALL bulleted elements contained within a box with a shaded border and at least 1 element in each box with an unshaded border is expected. |
Examination should include performance of ALL bulleted elements for at least 9 organ systems or body areas unless specific directions limit examination content. Note: Documentation of at least 2 bulleted elements for each area/system is expected. |
Medical decision making refers to the level of complexity associated with establishing a diagnosis and/or selecting a management option. The level of complexity is measured by the following factors:
• Number of Diagnoses or Management Options -- the number of possible diagnoses and/or the number of management options that must be considered by the examiner.
• Amount and/or Complexity of Data to Be Reviewed -- the amount and complexity of medical records, diagnostic tests, and/or other information that must be obtained, reviewed, and analyzed by the examiner.
• Risk of Significant Complications, Morbidity, and/or Mortality -- the risk of significant complications, morbidity, and/or mortality as well as comorbidities associated with the patient’s presenting problem(s), the diagnostic procedure(s) ordered, and/or the possible management options selected by the examiner.
2/3 elements must be met or exceeded:
Number of Diagnoses or Management Options |
Amount and/or Complexity of Data to Be Reviewed |
Risk of Complications, Morbidity, and/or Mortality |
Decision Making Level |
Minimal |
Minimal or None |
Minimal |
Straightforward |
Limited |
Limited |
Low |
Low Complexity |
Multiple |
Moderate |
Moderate |
Moderate Complexity |
Extensive |
Extensive |
High |
High Complexity |
Note: Levels for two out of three Medical Decision Making elements (i.e., Number of Diagnoses or Management Options, Amount and/or Complexity of Data to Be Reviewed, and Risk of Complications, Morbidity, and/or Mortality) must meet or exceed the requirements specified for each level of Medical Decision Making (i.e., Straightforward, Low Complexity, Moderate Complexity, or High Complexity).
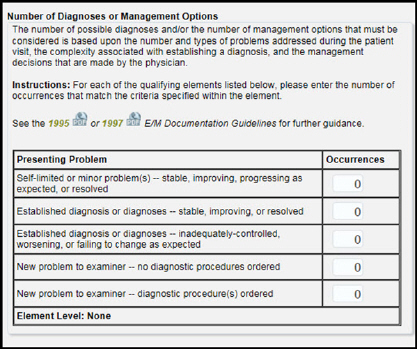
The number of possible diagnoses and/or the number of management options that must be considered is based upon the number and types of problems addressed during the patient visit, the complexity associated with establishing a diagnosis, and the management decisions that are made by the physician.
There are four possible levels of Number of Diagnoses or Management Options:
• Minimal
• Limited
• Multiple
• Extensive
Your entries in the Number of Diagnoses or Management Options subsection should be based on the documentation contained within the patient’s medical record that describes the patient’s presenting problem(s) including:
• Overall description -- (e.g., new, self-limiting, minor)
• Diagnosis -- (e.g., new, established)
• Current status -- (e.g., stable, improving, inadequately controlled, worsening, resolved)
• Diagnostic procedure(s) ordered
Note: A patient may have more than one presenting problem, and different criteria may apply to each. For example, a patient may have an established diagnosis of asthma that is stable; however, they may have recently taken a fall (the reason for the visit), and the physician may decide to order an X-ray to ascertain the severity of the patient’s injury:
Tip: Users should enter the number of occurrences that match the criteria specified in each option.
Once you have made your entry or entries in the Number of Diagnoses or Management Options subsection, the E/M interactive worksheet will automatically calculate the appropriate element level based on your entries within the subsection and your preferred set of guidelines.
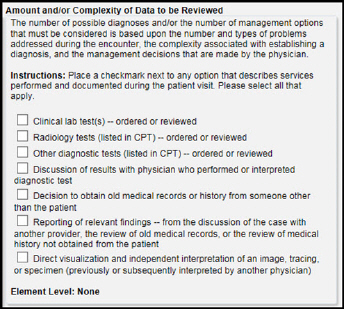
The amount and complexity of data to be reviewed is based on the types of diagnostic testing ordered or reviewed. A decision to obtain and review old medical records and/or obtain history from sources other than the patient increases the amount and complexity of data to be reviewed.
There are four possible levels of Amount and/or Complexity of Data to Be Reviewed:
• Minimal or None
• Limited
• Moderate
• Extensive
Your selections in the Amount and/or Complexity of Data to Be Reviewed subsection should be based on the documentation contained within the patient’s medical record that substantiates:
• Diagnostic tests ordered or reviewed
• Discussion of test results with the performing/interpreting physician
• Reporting of relevant findings from the discussion of the case with another provider
• Independent interpretations of a test previously or subsequently interpreted by another physician
• Decision by the physician to obtain old medical records or history from someone other than the patient.
Tip: Users should place a checkmark next to any option that describes services performed and documented during the patient visit.
Once you have made your selection(s) in the Amount and/or Complexity of Data to Be Reviewed subsection, the E/M interactive worksheet will automatically calculate the appropriate element level based on the options selected within the subsection and your preferred set of guidelines.
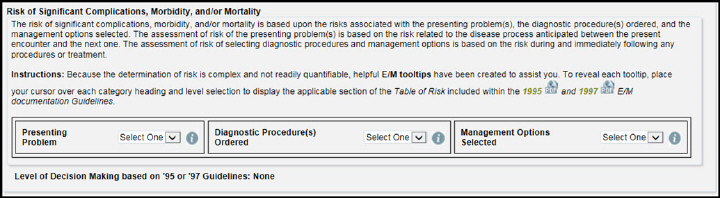
The risk of significant complications, morbidity, and/or mortality is based upon the risks associated with the presenting problem(s), the diagnostic procedure(s) ordered, and the management options selected. The assessment of risk of the presenting problem(s) is based on the risk related to the disease process anticipated between the present encounter and the next one. The assessment of risk of selecting diagnostic procedures and management options is based on the risk during and immediately following any procedures or treatment.
There are four possible levels of Risk of Significant Complications, Morbidity, and/or Mortality:
• Minimal
• Low
• Moderate
• High
You may click the “i” next to each drop-down menu to view a corresponding table associated with the presenting problem, diagnostic procedure(s) ordered, and management options selected.
Your selections in the Risk of Significant Complications, Morbidity, and/or Mortality subsection should be based on those details contained within the patient’s medical record that describe the nature of the presenting problem, the diagnostic procedures ordered, and management options selected. Since the determination of risk is complex and not readily quantifiable, use your cursor to reveal E/M Tooltips that will help you quantify the level of risk associated with each quantifying element.
Note: The highest qualifying element will determine the final level of risk.
Level |
Presenting Problem |
Diagnostic Procedure(s) Ordered |
Management Options Selected |
Minimal |
• One self-limited or minor problem ( e.g., cold, insect bite) |
• Laboratory tests requiring venipuncture • Chest X-rays • EKG/EEG • Urinalysis • Ultrasound • KOH prep |
• Rest • Gargles • Elastic Bandages • Superficial dressings |
Low |
• Two or more self-limited or minor problems • One stable chronic illness (e.g., well-controlled hypertension, non-insulin dependent diabetes) • One acute uncomplicated illness or injury (e.g., cystitis, sprain |
• Physiologic tests not under stress (e.g., pulmonary function tests) • Non-cardiovascular imaging studies with contrast (e.g., barium enema) • Superficial needle biopsies • Clinical laboratory tests requiring arterial puncture • Skin biopsies |
• Over-the-counter drugs • Minor surgery with no identified risk factors • Physical therapy • Occupational therapy • IV fluids without additives |
Moderate |
• One or more chronic illnesses with mild exacerbation, progression, or treatment side effects • Two or more stable chronic illnesses • Undiagnosed new problem with uncertain prognosis • Acute illness with systemic symptoms (e.g., pneumonitis, colitis) • Acute complicated injury (e.g., head injury with brief loss of consciousness) |
• Physiologic tests under stress (e.g., cardiac stress test, fetal contraction stress test) • Diagnostic endoscopies with no identified risk factors • Deep needle or incisional biopsy • Cardiovascular imaging studies with contrast AND no identified risk factors (e.g., arteriogram, cardiac catheterization) • Obtain fluid from body cavity (e.g., lumbar puncture, thoracentesis, culdocentesis) |
• Minor surgery with identified risk factors • Elective major surgery (open, percutaneous, or endoscopic) with no identified risk factors • Prescription drug management • Therapeutic nuclear medicine • IV fluids with additives • Closed treatment of fracture or dislocation without manipulation |
High |
• One or more chronic illnesses with severe exacerbation, progression, or treatment side effects • Acute or chronic illnesses or injuries that may pose a threat to life or bodily function (e.g., pulmonary embolus, severe respiratory distress, psychiatric illness with potential threat to self or others) • An abrupt change in neurologic status (e.g., seizure, TIA, sensory loss) |
• Cardiovascular imaging studies with contrast AND with identified risk factors • Cardiac electrophysiological tests • Diagnostic Endoscopies with identified risk factors • Discography |
• Elective major surgery (open, percutaneous, or endoscopic) with identified risk factors • Emergency major surgery (open, percutaneous, or endoscopic) • Parenteral controlled substances • Drug therapy requiring intensive monitoring for toxicity • Decision not to resuscitate or to de-escalate care because of poor prognosis |
Once you have made your selections in the Risk of Significant Complications, Morbidity, and/or Mortality subsection, the E/M interactive worksheet will automatically calculate the appropriate Medical Decision Making level based on your entries in all three subsections and preferred set of guidelines.
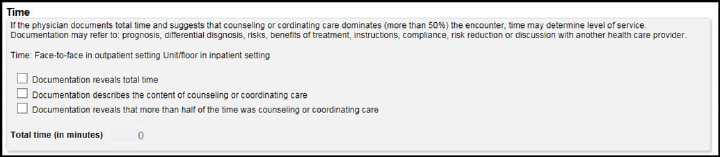
If the physician documents total time and suggests that counseling or coordinating care dominates (more than 50%) the encounter, time may determine level of service. Documentation may refer to: prognosis, differential diagnosis, risks, benefits of treatment, instructions, compliance, risk reduction or discussion with another health care provider.
You can make your selection and also enter the total time (in minutes).
Once you have made all of your selections, the E/M interactive worksheet will automatically calculate a suggested E/M code based upon your entries and preferred set of guidelines:
Tip: If the E/M interactive worksheet does not calculate a suggested E/M code, please check to ensure that you have completed all required sections of the worksheet.
After you have completed your E/M session, you have the following options:
• Use the Clear Worksheet button to clear your entries and begin a new session.
• Use the Print Worksheet button to print a copy of your completed worksheet to include within the medical record.
Tip: You may use your copy of Adobe Acrobat ® to print an electronic copy of your completed worksheet.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.