Home ►
EM ►
Part B Fact Sheet: Observation care services
Last Modified: 4/10/2024
Location: FL, PR, USVI
Business: Part A, Part B
Observation care is a well-defined set of specific, clinically appropriate services, which include ongoing short-term treatment, assessment, and reassessment, furnished while a decision is being made regarding whether a patient will require further treatment as a hospital inpatient or if they are able to be discharged from the observation care. Outpatient observation services are commonly ordered for patients who present to the emergency department and then require a significant period of treatment or monitoring to make a decision concerning their admission or discharge.
Note: Observation services are not medically necessary when determined by the facility’s standard operating procedure or protocol for a given diagnosis or service.
Outpatient observation services generally do not exceed 24 hours. The decision to either discharge a patient from the outpatient observation care or to admit the patient as an inpatient can be made in less than 48 hours, usually in less than 24 hours.
Although some patients may require a second day of outpatient observation, only in rare and exceptional cases do outpatient observation services span more than 48 hours.
The order for outpatient observation services must be in writing and clearly specify outpatient observation. The order must include the reason for observation, services ordered and be signed, dated and timed by the physician responsible for the patient during his/her outpatient observation care.
Verbal orders are permitted but must be documented by the individual receiving the order. The ordering practitioner must review and confirm the verbal order when they see the patient.
Note: Verbal orders should be the exception; not the rule.
Only the practitioner who orders and is responsible for the patient’s care while receiving outpatient observation services, can bill the outpatient observation care CPT codes.
As of January 1, 2023, for most E/M visit families, practitioners will select visit level based on the level of medical decision making (MDM) or the amount of time spent by the physician or non-physician practitioner. For all E/M visits, history and physical exam must be performed in accordance with code descriptors, but history and exam no longer impact visit level selection. When practitioner time is used to select visit level, the full time must be completed; the general CPT rule regarding the midpoint for certain timed services does not apply.
Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of an E/M visit code. It would not be medically necessary or appropriate to bill a higher level of E/M service when a lower level of service is warranted. The volume of documentation should not be the primary influence upon which a specific level of service is billed. Documentation should support the level of service reported.
For dates of service prior to January 1, 2023, observation services are billed by the practitioner who orders and is responsible for the patient’s care while receiving outpatient observation services using:
Initial observation care: 99218-99220
Subsequent observation care: 99224-99226
Discharge: 99217
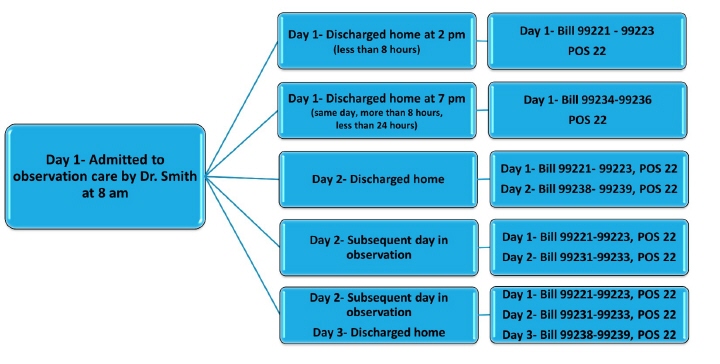
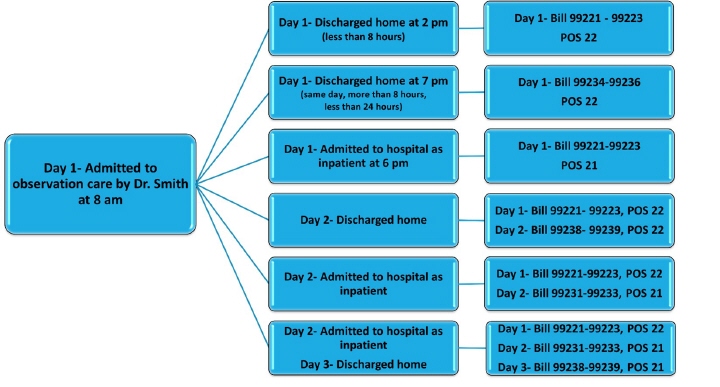
Starting in CY 2023, observation care by practitioners is billed using the same CPT codes as hospital inpatient care, CPT codes 99221-99223, 99231-99239.
For dates of service on and after January 1, 2023, observation services are billed by the admitting physician using:
Initial hospital inpatient or observation care: 99221-99223
Subsequent hospital inpatient or observation care: 99231-99233
Hospital Inpatient or Observation Care Services (Including Admission and Discharge Services): 99234-99239
Hospital Inpatient or Observation Discharge Services: 99238-99239
Observation care codes are billed only by the treating physician. All other practitioners who provide consultations or additional evaluations or services while the patient is receiving hospital observation services bill office and other outpatient visits, codes 99202-99205 or 99211-99215. The new vs. established patient rules apply.
The time counted toward the hospital inpatient and observation care codes is “per day” also referred to as "date of encounter" which means "calendar date". Practitioners will select a code that reflect all services provided in all sites on the date of service.
Observation care is an outpatient service. Although the code range includes inpatient and outpatient services, the place of service code should identify the patient's location for the service billed. Claims for observation care are typically billed with place of service code (POS) -22 (outpatient hospital).
Observation admission and discharge, same day
If a patient is admitted to outpatient observation care and discharged later the same calendar day, the observation admission including discharge codes may be applicable. Initial observation including discharge care on the same date of service may be billed using codes 99234-99236 if the care involves 8 hours, but less than 24 hours. The place of service code should identify the patient's location as outpatient for the service billed.
The medical record must include documentation stating the stay for observation care involves at least 8 hours and less than 24 hours on the same calendar date. The documentation must also include dated and timed physician orders regarding the care the patient is to receive, nursing notes, progress notes prepared by the physician while the patient received observation services. The physician must also document the care provided, which includes the admission and discharge were both personally performed by the physician in person.
Note: Hours are based on a calendar day.
The observation discharge, CPT code 99217, cannot also be reported for this scenario.
Observation to inpatient, same day
A transition from outpatient observation care to inpatient status does not constitute a new stay. Initial and subsequent hospital or observation care codes may not be billed for observation services provided on the same date the physician admits the patient as an inpatient.
If the patient is admitted as an inpatient by the same physician, or physician of the same specialty in the same group practice, on the same day as the observation admission, bill only one initial hospital inpatient or observation care code 99221-99223 for the inpatient admission. Medicare payment for the hospital inpatient or observation care codes include all services provided to the patient by the same physician on the date of admission regardless of the site of service. The place of service code should identify the patient's location as inpatient (pos 21) for the service billed.
Observation to inpatient, next or subsequent day
For services on and after January 1, 2023, the initial observation service is billed by the admitting physician using the initial hospital inpatient or observation care codes, 99221-99223. The place of service code should identify the patient's location as outpatient for the service billed.
Although the patient is admitted to the hospital as an inpatient on the next or subsequent calendar date, the transition from outpatient observation care to inpatient status does not constitute a new stay.
If the patient is admitted by the same physician, or physician of the same specialty in the same group practice, as an inpatient on the next or subsequent day following an outpatient observation care day, bill a subsequent hospital inpatient or observation care code, 99231-99233 for the hospital admission. The POS code should identify the patient's location as inpatient (POS 21) for the service billed.
The Hospital Inpatient or Observation Discharge Day Management service, CPT codes 99238 or 99239, are not reported for this scenario.
If a patient is admitted to inpatient hospital care or is in observation care and then discharged on a different calendar date, the physician may report both the Initial Hospital Inpatient or Observation Care, CPT codes 99221-99223 and the Hospital Inpatient or Observation Discharge Day Management service, CPT code 99238 or 99239 for the date of the encounters.
If the patient is receiving observation care on three different calendar days, the physician may report Day 1- the Initial Hospital Inpatient or Observation Care, CPT codes 99221-99223, Day 2- the Subsequent Hospital Inpatient or Observation Care: 99231-99233 and Day 3- the Hospital Inpatient or Observation Discharge Day Management service, CPT code 99238 or 99239 for the date of the encounters.
Note: Only in rare and exceptional cases do outpatient observation services span more than 48 hours.
Observation services may be split (or shared) between a physician and non-physician practitioner in the same group practice. One of the practitioners must have face-to-face (in-person) contact with the patient, but it does not necessarily have to be the physician, nor the practitioner who performs the substantive portion and bills for the visit. The substantive portion can be entirely with or without direct patient contact, and is determined by the proportion of total time, not whether the time involves patient contact.
The medical record must identify the physician and NPP who performed the visit, be signed and dated by the practitioner who performed the substantive portion of the visit. The service is billed by the practitioner who performed the substantive portion of the visit.
For calendar year 2023, the practitioner who spends more than half of the total time or performs the medically appropriate history or exam described in the code descriptor, or MDM can be considered to have performed the substantive portion and can bill for the split (or shared) E/M visit. The provider who performs the substantive portion of the visit using one of the three key components as the substantive portion in 2023 must perform and document that component in its entirety as described in the code descriptor.
When using time, only distinct time can be counted. If both practitioners meet to discuss the patient, only the time of one of the practitioners can be counted.
Modifier -FS must be reported on claims to identify the service was a split (or shared) visit.
Starting in 2024, the substantive portion is determined by the physician or NPP who furnished more than half of the combined total time.
Note: Services billed by the non-physician practitioner are reimbursed at 85% of the physician fee schedule.
In addition to meeting the documentation requirements for a medically appropriate history or examination, and medical decision-making documentation, the physician's documentation must satisfy the E/M guidelines for admission and discharge from observation or hospital care. The medical record should indicate the billing practitioner was physically present and personally performed the service; they personally authored the order, progress notes, and discharge notes.
Note: The medical record is expected to demonstrate the consistency between the practitioner order, the services provided, and the medical necessity of those services, including the medical appropriateness of the observation stay.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.