Last Modified: 4/20/2024
Location: FL, PR, USVI
Business: Part B
Effective January 1, 2017, the JW modifier has been required on all claims for drugs and biologicals (hereafter, drug) separately payable under Medicare Part B with unused and discarded amounts (hereafter, discarded amounts) from single-dose containers or single-use packages (hereafter, single-dose containers). Providers must document the amount of discarded drugs in the beneficiary’s medical record.
Medicare has observed low compliance with providers using the JW modifier. This leads to incomplete JW modifier data which discarded drug refund amounts rely on. CMS established that a separate modifier, the JZ modifier, will be required on claims for single-dose container drugs to attest when there are no discarded amounts no later than July 1, 2023.
Effective July 1, 2023, providers and suppliers are required to report the JZ modifier on all claims that bill for drugs from single-dose containers that are separately payable under Medicare Part B when there are no discarded amounts.
In general, the JW and JZ modifier policy applies to all drugs separately payable under Medicare Part B described as supplied in a “single-dose” container based on FDA-approved labeling or product information and is not otherwise excluded.
• Wound care or cellular and/or tissue-based products for skin wounds that meet the definition of a refundable single source and single-dose drug or biological (see above) are subject to billing using the JW and JZ modifier, as appropriate (
November 18, 2023 Federal Register/Vol.87, No 222, page 69722)

.
The JW and JZ modifiers are mostly reported on claims from the physician’s office and hospital outpatient settings for beneficiaries who receive drugs incident to physicians’ services. The JW and JZ modifier requirements also apply to Critical Access Hospitals (CAHs).
JW Modifier: A HCPCS Level II modifier required to be reported on a claim to report the amount of drug that is discarded and is eligible for payment under the discarded drug policy. The modifier should only be used for claims that bill single-dose container drugs.
JZ Modifier: A HCPCS Level II modifier reported on a claim to attest that no amount of drug was discarded and is eligible for payment. The modifier should only be used for claims that bill for single- dose container drugs.
Modifier |
Short descriptor |
Long descriptor |
Effective date |
JW |
Discarded drug not administered |
Drug amount discarded/not administered to any patient |
January 1, 2017 |
JZ |
Zero drug wasted |
Zero drug amount discarded/not administered to any patient |
July 1, 2023 (may begin using January 1, 2023) |
For drugs from a single-dose container:
• If you discard any of the drug, continue to report the JW modifier on the claim.
• If you did not discard any of the drug, report the JZ modifier on the claim starting on July 1, 2023.
JW and JZ modifiers are not used for claims that are:
• Not separately payable (i.e., packaged outpatient prospective payment system (OPPS) or ambulatory surgical center (ASC) drugs
• Administered in the federally qualified health center (FQHC) or rural health clinic (RHC) setting
• Overfilled amounts (any amount of drug greater than the amount identified on the package or label)
• Hospital inpatient admissions that are billed under the inpatient prospective payment system (IPPS)
• Influenza, pneumococcal, and COVID–19 vaccines
• Drugs from multiple-dose containers
Claim situation |
Dates of service |
Outcome |
Claims with discarded amounts that do not use the JW modifier |
Furnished between January 1, 2017, and June 30, 2023 |
Will be subject to review |
Claims not reported with the JW or JZ modifier |
Furnished on or after July 1, 2023 |
May be subject to provider audits |
Claims that do not report the appropriate modifiers |
On or after October 1, 2023 |
May be returned as unprocessable/rejected. Resubmit claim with modifier |
When a provider must discard the remainder of a single-dose container after administering a dose/quantity of the drug to a Medicare patient, the Medicare Part B program provides payment for the amount of drug discarded as well as the dose administered, up to amount of the drug as indicated on the container or package label.
CMS encourages physicians, hospitals and other providers and suppliers to care for and administer to patients in such a way that they can use drugs most efficiently.
When you administer a separately payable drug under Medicare Part B from a single-dose container and there are discarded amounts, you must file a claim with two lines:
First claim line (for the administered amount) must include:
• HCPCS code for drug given
• No modifier
• Number of units administered in the unit field
• Calculated submitted price for only the amount of the drug given
Second claim line (for the discarded amount) must include:
• HCPCS code for drug given
• JW modifier to indicate waste
• Number of units discarded in the unit field
• Calculated submitted price for only the amount of the drug waste
Documentation must clearly indicate the number of units administered and amount discarded in the patient's medical record.
When you administer a separately payable drug under Medicare Part B from a single-dose container and there are no discarded amounts, file a claim on one detail line using the JZ modifier.
Claim line must include:
• HCPCS code for drug given
• JZ modifier to indicate no waste
• Number of units administered in the unit field
• Calculated submitted price for the amount given
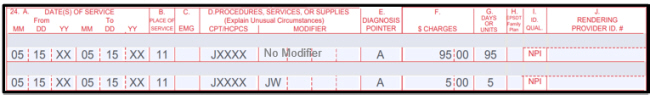
JW modifier billing example
A provider or supplier uses a single-dose container that is labeled to contain 100 mg of a drug to administer 95 mg to the patient and 5 mg are discarded. The drug dose description is 1 mg per unit. The 95 mg dose is billed on one line, with the calculated submitted price for only the amount of the drug given, while the discarded 5 mg must be billed on another line with the JW modifier with the calculated submitted price for only the amount of the drug wasted. Both line items would be processed for payment.
Drug code - JXXXX
Single-dose container - 1 mg = 1 unit
Labeled - 100 mg
95 mg administered
5 mg discarded
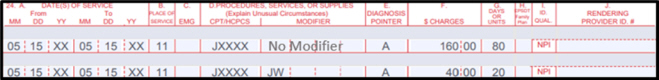
More than one vial
When more than one single-dose container is used to administer the required dose and there are discarded amounts, file the claim using two detail lines.
For example, if two vials labeled as containing 50 mg are used to prepare a prescribed dose of 80 mg of a drug (assuming that each billing unit is 1 mg), the claim should be billed on two lines: the first line should include the billing and payment code, no modifier, and 80 billing units and the second line should include the billing and payment code, the JW modifier, and 20 billing units.
Drug code - JXXXX
Single-dose container - 1 mg = 1 unit
Labeled - 50 mg X 2 vials = 100
80 mg administered
20 mg discarded
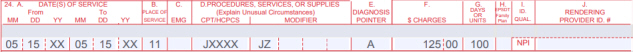
JZ modifier billing example
A provider or supplier uses a single-dose container that is labeled to contain 100 mg of a drug to administer all 100 mg with nothing discarded. The drug dose description is 1 mg per unit. The claim line should be billed on one line showing the 100 mg dose using the JZ modifier attesting that there were not discarded amounts.
Drug code - JXXXX
Single-dose container - 1 mg = 1 unit
Labeled - 100 mg
100 mg administered
Zero discarded
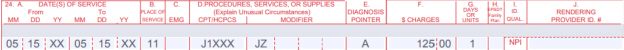
Billing examples without JW modifier
JW modifier is not permitted when the actual dose of the drug administered is less than the HCPCS billing unit. In this situation, the billing provider or supplier would report administering the full billing unit along with the JZ modifier.
Example 1:
Drug J1XXX = One billing unit is equal to 10 mg of the drug in a single-dose container.
• 7 mg dose was administered to the patient while 3 mg of the drug was discarded.
• 7 mg dose is billed using one billing unit representing 10 mg on a single line item. Report the JZ modifier on this line.
• Single line item of one (1) unit would be processed for payment of 10 mg of drug administered and discarded.
• Billing another unit on a separate line item with the JW modifier for the discarded 3 mg of drug is not permitted and would result in an overpayment.
• Medicare record must clearly indicate the number of units administered and amount discarded.
Drug code J1XXX
Single-dose container = 10 mg
7 mg administered
3 mg discarded
Example 2:
Drug J12XX = One billing unit is equal to 1 mg of the drug in a single-dose container.
• 3.5 mg dose of the drug was administered to the patient using four units representing 4 mg, while 0.5 mg of the drug was discarded. Report the JZ modifier on this line.
• Single line item of four (4) units would be processed for payment of 4 mg of drug administered and discarded.
• Billing another unit on a separate line item with the JW modifier for the discarded 0.5 mg of drug is not permitted and would result in an overpayment.
• Medicare record
must clearly indicate the number of units administered and amount discarded.
Drug code = J12XX
Single-dose container = 1 mg
3.5 mg administered
0.5 mg discarded
The JW and JZ modifiers are required to be reported for drugs from single-use containers billed with a NOC code (for example, J3490, J3590, C9399).
The JW and JZ modifiers apply to any separately payable single-dose drugs administered in the ESRD setting that are not renal dialysis service drugs or biological products provided for the treatment of ESRD and are billed using the AY modifier. Either the JW or JZ modifier is reported in conjunction with the AY modifier. In such cases, the billing provider should report the AY modifier on a single claim line along with the JZ modifier or when there are discarded amounts, on the two claim lines used for the drug.
The JW and JZ modifier requirement applies to all separately payable drugs assigned payment indicator “K2” (Drugs paid separately when provided integral to a surgical procedure on ASC list; payment based on OPPS rate) in the ASC for which there is a discarded amount.
Does not apply assigned payment indicator “N1” (Packaged service/item; no separate payment made) under the ASC payment system.
References:
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.



 .
.