Last Modified: 2/23/2024
Location: FL, PR, USVI
Business: Part B
The CMS claims processing system has a limit for the total dollar amount submitted per claim. The total digits that can be accepted on a claim is seven. The
Standard Companion Guide for Health Care Claim: Professional (837P) 
clarifies and specifies data content when exchanging transactions electronically with Medicare. One of the general rules pertaining to an 837P (Part B electronic claim) transaction is the maximum number of characters submitted in any dollar amount field is seven characters. When claim amounts exceed seven digits, the claim must be split into two when billing for dollar amounts above $99,999.99.
First Coast has seen an increase in claims for drugs,
hemophilia clotting factors, and
skin substitutes that exceed the dollar amounts above $99,999.99. Multiple claims with modifier 76 which are submitted separately due to having a dollar amount exceeding $99,999.99 are currently being denied. Effective for claims received on or after November 6, claims missing the required information will be rejected.
When billing two claims (or three or more claims when appropriate) ensure that your total dollar amounts are different on each claim. Use modifier 76 to indicate repeat service on the subsequent claim(s) and notate in the narrative why the claim is split this way. This will prevent the system from assuming the claims are an exact duplicate.
Submit separate claims as follows:
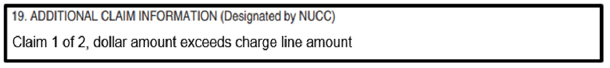
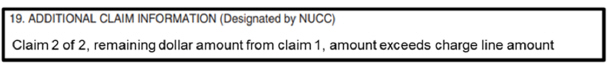
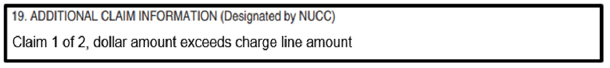
Claim 1
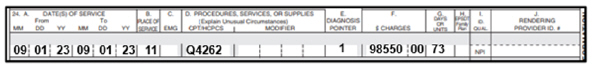
• Submit the service with an acceptable dollar amount (less than $99,999.99)
• Do not use dollar signs, decimals, dashes, or commas for dollar amounts
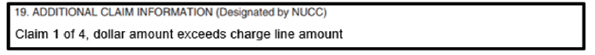
• In the narrative field, identify as "Claim 1 of 2, dollar amount exceeds charge line amount."
• Item 19 of the CMS 1500 claim form or loop 2400 (line note), segment NTE02 (NTE01=ADD) for electronic claims
• Note: An appropriate administration code can be billed on the first or second claim, not both, for drug billing.
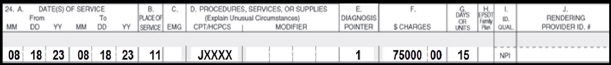
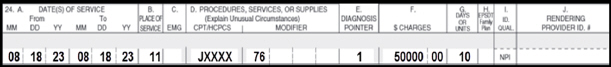
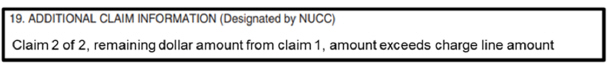
Claim 2
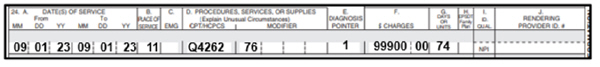
• Enter the charge as the remaining dollar amount from the total split
• Append modifier 76 to indicate repeat service
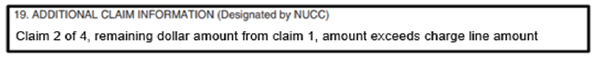
• In the narrative field, identify as, "Claim 2 of 2, remaining dollar amount from claim 1 amount exceeds charge line amount."
When splitting into three claims, use the following verbiage for the narratives:
• Claim 1 of 3, dollar amount exceeds charge line amount (on the first claim).
• Claim 2 of 3, remaining dollar amount from claim 1, amount exceeds charge line amount (on the second claim).
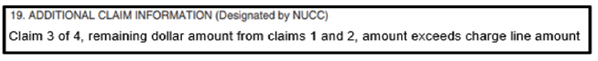
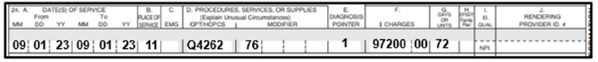
• Claim 3 of 3, remaining dollar amount from claims 1 and 2, amount exceeds charge line amount.
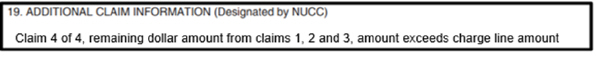
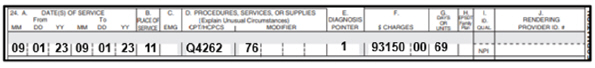
If you have more than three claims, ensure the narrative follows the verbiage like the above narratives, ensuring to indicate claim X out of X, remaining dollar amount from claim(s) x, amount exceed charge line amount.
Billing example 1: The patient received 25 mgs of JXXXX for a total billed amount of $125,000.00. The unit of service is based on 1 mg. Based on the dollar amount two separate claims need to be submitted.
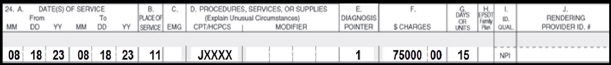
Claim one:
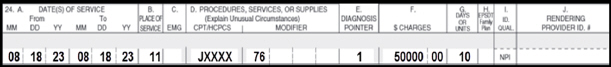
Claim two:
Billing example 2: The patient received 288 sq cm of Q4262 for a total billed amount of $388,800.00. The unit of service is based on 1 sq cm. Based on the dollar amount four separate claims need to be submitted.
Claim one:
Claim two:
Claim three:
Claim four:
Please be sure to use these instructions to bill these types of claims correctly and prevent claim rejections.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.



 clarifies and specifies data content when exchanging transactions electronically with Medicare. One of the general rules pertaining to an 837P (Part B electronic claim) transaction is the maximum number of characters submitted in any dollar amount field is seven characters. When claim amounts exceed seven digits, the claim must be split into two when billing for dollar amounts above $99,999.99.
clarifies and specifies data content when exchanging transactions electronically with Medicare. One of the general rules pertaining to an 837P (Part B electronic claim) transaction is the maximum number of characters submitted in any dollar amount field is seven characters. When claim amounts exceed seven digits, the claim must be split into two when billing for dollar amounts above $99,999.99.