Guía de ayuda - Gateway de reapertura de reclamación
Bienvenido a la Guía de ayuda del Gateway de reapertura de reclamación de First Coast. El Gateway de reapertura de reclamación es una herramienta interactiva que no requiere inscripción ni registro, y ofrece una manera fácil de hacer correcciones a reclamaciones de la Parte B directamente en la página web de First Coast. Aunque la herramienta está diseñada para copiar el proceso de reapertura de reclamación en el Secure Provider Online Tool (SPOT) de First Coast, este Gateway puede ser utilizado pro cualquier proveedor, sin importar si están o no inscritos en SPOT. El único requisito que se necesita para usar el Gateway es tener acceso a la internet y validar el proveedor utilizando el Identificador de Proveedor Nacional (NPI); el Número de Acceso de Transacción del Proveedor (PTAN); y los últimos cinco dígitos del Número de Identificación Fiscal (TIN).
Aviso: Por favor tenga su remesa de pago a la mano para referirse a detalles de la reclamación mientras use el gateway.
Entrando al gateway
Mientras esté en la página web de First Coast, navegue sobre la opción de Reclamaciones y EDI en la barra de navegación superior, luego vaya al icono de Gateway de reaperturas ubicado en la fila inferior.
Usando el gateway
Una vez usted haya navegado al gateway, haga clic en el botón de Aceptar (“Accept”) en la pantalla de Relevo de responsabilidad. Entonces usted podrá ver la página de verificación del proveedor:

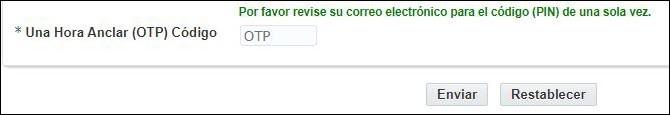
1. Escriba su NPI, PTAN, y los últimos cinco dígitos de su TIN. Entonces, seleccione su estado, escriba una dirección de correo electrónica válida, y haga clic en el botón de “Código OTP de correo electrónico”. Usted recibirá rápidamente un correo electrónico con lo siguiente en la línea de asunto: “URGENTE: Acceso al Gateway de reaperturas” que contiene su código.
2. Escriba su código en el encasillado PIN de un solo uso (OTP) que aparece luego de hacer clic en “Código OTP de correo electrónico.” Luego, haga clic en “Enviar.”
3. Luego, aparecerá la pantalla de búsqueda de reclamación. Escriba el número interno de reclamación (ICN) y el ID de beneficiario de Medicare.
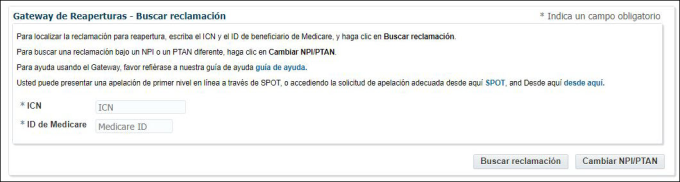
Haga clic en “Buscar reclamación” y el gateway automáticamente determinará si algunos ítems de línea son elegibles para una reapertura. Usted también puede regresar a la pantalla previa si usted necesita buscar por una reclamación bajo un proveedor diferente al hacer clic en el botón de “Cambiar NPI / PTAN”.
AVISO: Si la reclamación no es elegible para una reapertura, un mensaje de error aparecerá, y usted puede hacer clic en “Solicitud de apelación” para ser llevado a la página de formularios de apelaciones en la página web. Vea más información acerca de los códigos de modificadores y procedimientos restringidos que aplican a este gateway, los cuales son los mismos para presentaciones de SPOT. Además, si la reclamación ha sido devuelta como no procesable, ya ha sido ajustada, o ha sido archivada como no asignada, no es elegible para ser reabierta a través del gateway.
4. Una vez el gateway ha determinado que su reclamación es elegible para una reapertura, aparecerán las líneas elegibles asignadas de la reclamación. En la línea que usted desea corregir, seleccione su tipo de solicitud del menú desplegable de Tipo de Solicitud y escriba los datos que usted desea cambiar en su reclamación. Luego haga clic en “Enviar”:
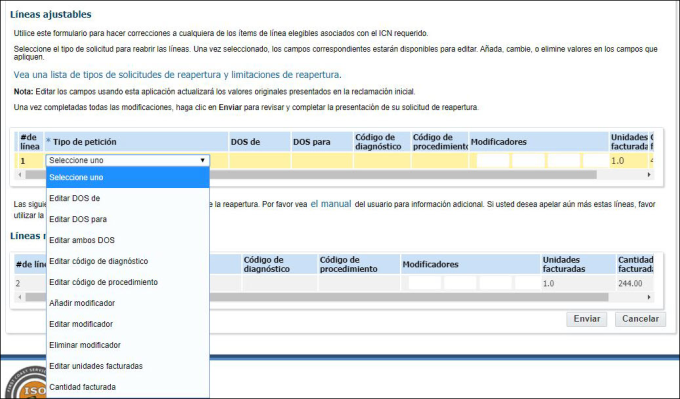
Los tipos de solicitud disponibles son:
- Editar DOS de
- Editar DOS para
- Editar ambos DOS
- Editar código de diagnóstico
- Editar código de procedimiento
- Añadir modificador
- Editar modificador
- Eliminar modificador
- Editar unidades facturadas
- Cantidad facturada
Tipos de solicitud adicionales:
- Facturado por error
- Informe una reclamación completa o líneas individuales de una reclamación como facturadas por error. La reclamación debe pagarse total o parcialmente y no debe tener información del pagador secundario de Medicare para poder utilizar esta función.
- Corrección de historial
- Esta opción le permite volver a enviar una reclamación sin hacer ninguna corrección. Esta opción solo es válida para los siguientes escenarios:
- El expediente del beneficiario se ha corregido para indicar que Medicare ahora es el principal para la (s) fecha (s) de servicio de la reclamación denegada.
- El expediente del beneficiario se ha corregido para indicar que el beneficiario tiene derecho a la Parte B de Medicare para la (s) fecha (s) de servicio de la reclamación rechazada.
- El expediente del beneficiario se ha corregido para indicar que el período de elección del hospicio del beneficiario ya no entra en conflicto con la (s) fecha (s) de servicio de la reclamación denegada.
- El expediente del beneficiario se ha corregido para indicar que el beneficiario ya no está cubierto por un Plan Medicare Advantage para las fechas de servicio en la reclamación denegada.
- Denegaciones de ediciones médicamente improbables (MUE) que involucran dos reclamaciones que se presentaron al mismo tiempo; resultando en una denegación de MUE junto con una denegación de una reclamación duplicada.
- Esta opción le permite volver a enviar una reclamación sin hacer ninguna corrección. Esta opción solo es válida para los siguientes escenarios:
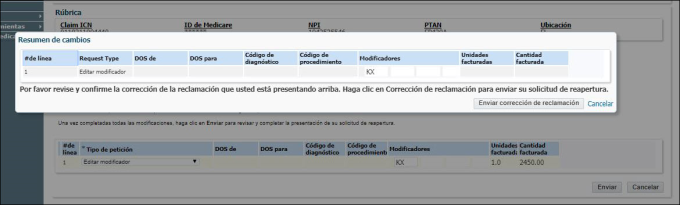
AVISO: Ver más instrucciones, comentarios, y limitaciones para tipos de solicitud aquí.
5. Luego de hacer clic en “Enviar,” aparecerá una pantalla de resumen de cambios. Revíselos para exactitud, y si son aceptables, haga clic en el botón de “Enviar corrección de reclamación”. Si no son exactos, haga clic en “Cancelar” y usted regresará a la página de líneas ajustables para hacer cualquier corrección necesaria. Una vez usted haya hecho sus correcciones, haga clic en “Enviar” de nuevo y revise el resumen de cambios. Si los cambios son aceptables, haga clic en “Enviar corrección de reclamación”.
6. Aparecerá una pantalla de confirmación. Usted puede hacer clic en “Imprimir”o “Corrección a Nueva Reclamación”:
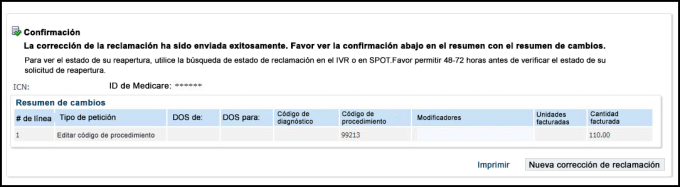
7. Si usted tiene más reclamaciones para reabrir, haga clic en el botón de “Corrección a Nueva Reclamación” y el gateway lo devolverá a usted a la página de búsqueda de reclamaciones, donde usted puede escribir el próximo ICN y el ID de Medicare. Si las reclamaciones no son para el mismo proveedor, haga clic en el botón de “Cambiar NPI / PTAN” para regresar a la página de verificación de proveedor para escribir la información del nuevo proveedor.
AVISO: Usted puede verificar el estado de su reapertura usando el sistema de respuesta automática (IVR) o SPOT. Por favor permita de 48-72 horas antes de verificar el estado.