The SPOT User Guide: Section 4 - MBI Lookup
Providers must use the patient’s Medicare Beneficiary ID (MBI) for all transactions. Per CMS MBI education, there are three ways to obtain MBIs. This MBI Lookup tool is one of those options. The MBI is confidential and should be protected as Personally Identifiable Information (PII) and used only for Medicare related business. CMS requires specific data elements, including the beneficiary’s social security number to obtain the MBI.
When using the MBI Lookup feature, you must adhere to the HIPAA Eligibility Transaction System (HETS) Rules of Behavior. As a reminder, the rules clearly state that HETS is for enrolled Medicare Fee-for-Service (FFS) health care providers and suppliers with a FFS electronic data interchange enrollment to submit Medicare claims to a Medicare Administrative Contractor. Submitters may not use HETS to verify eligibility or coverage for Medicare Advantage (Part C) or Medicare drug (Part D) plans. Any violations of the HETS Rules of Behavior may result in the possible referral of your organization for investigation.
To use the MBI Lookup, take the following steps:
- Select MBI Lookup from the top menu.

Figure 1: MBI Lookup Input
- Using the search tab on the left, complete the required fields (scroll down to view all fields):
- Beneficiary’s first name
- Last name
- SSN (social security number)
- Date of birth
- Beneficiary’s first name
-
Check the “I’m not a robot” box and follow the instructions (if any). When the green checkmark appears, click Search.
Note: reCAPTCHA must be enabled within the browser settings.
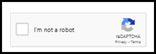
Figure 2: reCAPTCHA block
- Results will appear, showing the beneficiary’s first name, last name, and MBI.
Note: You can retrieve an MBI for a beneficiary up to four years from the beneficiary’s date of death.
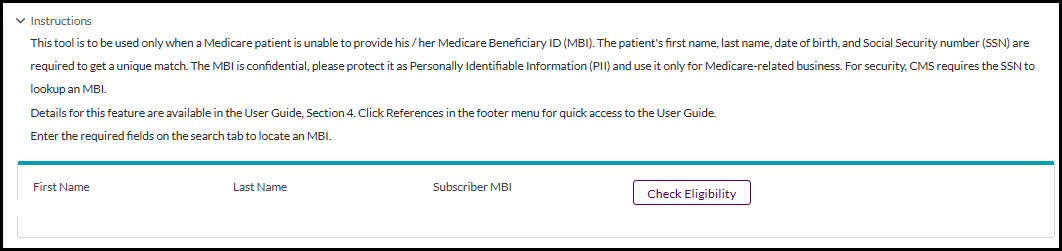
Figure 3: MBI Lookup Search Results
- Optional: click the Check Eligibility button to quickly access the eligibility screens for this beneficiary.