Ambulatory surgical center (ASC) prior authorization (PA) claim submission guidelines
Prior authorization (PA) for the ASC prior authorization demonstration is voluntary. However, if a provider elects to bypass PA, applicable ASC claims will be subject to prepayment medical review.
Once a prior authorization request (PAR) is submitted and reviewed, the ASC will receive a decision letter indicating if the PAR is affirmed, partially affirmed, or non-affirmed. The decision letter will contain a unique tracking number (UTN) that is required to be reported on the ASC facility place of service (POS) 24 claim. The PAR decision and UTN will be valid for a date of service performed within 120 days from the date of the decision.
Reporting the UTN on the claim
The UTN is required to be reported on the ASC facility POS 24 claim.
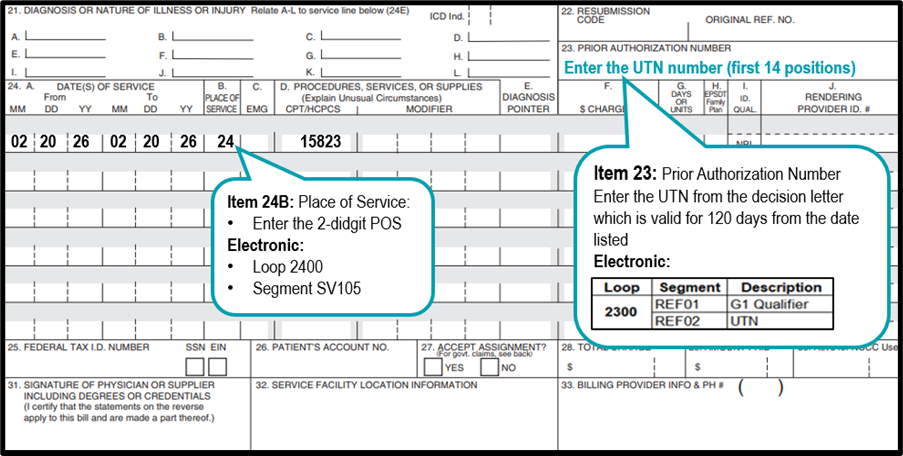
Report the UTN from the decision letter which is valid for 120 days from the date listed as follows on the ASC claim:
- Electronic claim in 2300 - Service Line loop in the Prior Authorization reference (REF) segment:
- REF01 = G1 qualifier
- REF02 = UTN
- CMS-1500 claim form in Item 23 in the first 14 positions
Example of reporting POS and UTN on the ASC facility claim:
Claims submitted with an affirmed decision on file
Claims submitted for PARs that received a provisional affirmation PA decision, including any service that was part of a partially affirmed decision, must include the UTN number listed on the decision letter.
If all Medicare coverage, coding, and payment requirements are met, the claim will likely be paid. Claims receiving a provisional affirmation may be denied based on either of the following:
- Technical requirements that can only be evaluated after the claim has been submitted for formal processing; or
- Information was not available at the time of a PAR.
Claims for which there is a provisional affirmation PA decision will be afforded some protection from future audits, both pre- and post-payment; however, review contractors may audit claims if potential fraud, inappropriate utilization, or changes in billing patterns are identified.
Claims submitted with a non-affirmed decision on file
A non-affirmed PAR decision is not an initial claim determination and is not appealable. However, a non-affirmation PAR decision does not prevent claim from being submitted. Remember a provider has an unlimited number of opportunities to resubmit a PAR if a claim has not yet been submitted and denied.
If a provider submits a claim for a non-affirmed PAR, the UTN from the decision letter must be reported on the claim. First Coast will deny claims submitted when the PA decision was non-affirmed. The claim denial is appealable.
For more information on appeals visit the CMS IOM Pub. 100-04 Medicare Claims Processing Manual, Chapter 29 or the First Coast appeals center.
No PA decision on file - Prepayment reviews
ASC claims submitted without a PA decision on file will be subject to a prepayment medical review. Prepayment medical record review means that the First Coast will make a claim determination before claim payment using the standard Medicare prepayment medical record review process.
ASCs do not need to do anything differently when submitting a claim without a UTN. They do not need to put any information in the remarks field or submit any unsolicited documentation at the time of claim submission.
First Coast will stop the claim prior to payment and send the ASC an additional documentation request (ADR):
- Letter is sent through the US Postal Service and/or electronically
- ASCs will have 45 days to respond to the ADR with all requested documentation through:
- SPOT portal
- Fax
- esMD
First Coast will have 30 days to review the documentation and render a claim determination:
- If approved, claim will process for payment.
- If not-approved, claim will denial and will have appeal rights.
Claims for associated and related services
Associated or related (professional) services will be denied when there was a non-affirmation PAR decision for the ASC service(s), or when the ASC facility claim was denied after prepayment review. These associated services include but are not limited to services such as anesthesiology services and/or physician services.
As part of this demonstration, ASC facility providers must report the UTN on their claim. Other billing providers or practitioners should submit their claims as usual and do not report a UTN; however, claims for associated or related services in this PA demonstration will not be paid if the service subject to PA or prepayment review is not eligible for payment.
Claim exclusions
The following claim types are excluded from the ASC PA demonstration:
- Veterans Affairs
- Indian Health Services
- Medicare Advantage
- Medicare Advantage sub-category IME only claims
- Railroad Retirement Board
Advanced beneficiary notice (ABN)
If the ASC receives a non-affirmed PA decision because the service was determined to be not medically reasonable and necessary, the provider should issue an ABN in advance of performing the service if it is expected that payment will be denied. The provider should submit the claim with the GA modifier appended to it. First Coast will determine the validity of the ABN in accordance with standard ABN policies.
If an applicable claim is submitted without a PA decision and a GA modifier (waiver of liability statement issued as required by payer policy) is reported on the claim, it will be stopped for additional documentation to be requested, and a review of the ABN will be performed (to determine the validity of the ABN) following standard claim review guidelines and timelines.
The provider should issue ABN and submit the claim with a GX modifier (notice of liability issued, voluntary under payer policy) if it is expected that Medicare would deny payment for a service under the statutory exclusion for purely cosmetic services. Under those circumstances, ABN is voluntary and is not required to bill the patient for the service that is denied under the cosmetic services exclusion. However, CMS encourages providers to issue an ABN in this situation to inform the beneficiary of the likelihood of financial liability.
For more information, review the CMS IOM Pub. 100-04 Medicare Claims Processing Manual, Chapter 30, section 40 or the First Coast Advance Beneficiary Notice of non-coverage article.
Medicare secondary situations
If the provider is seeking payment from Medicare as a secondary payer for an applicable ASC service, PA should be obtained. If all relevant Medicare coverage requirements are met for the item(s), then a provisional affirmative PA decision will be sent to the provider.
In situations where Medicare is the secondary payer, the provider will need to submit the claim to the primary insurance before submitting the claim to Medicare as secondary. The provider or beneficiary must include the UTN on the claim submitted to Medicare for payment or the claim will be stopped for prepayment review.