Life cycle of an enrollment application
There are many steps that must take place to process an enrollment application. The following chart provides a high-level progression of a basic enrollment:
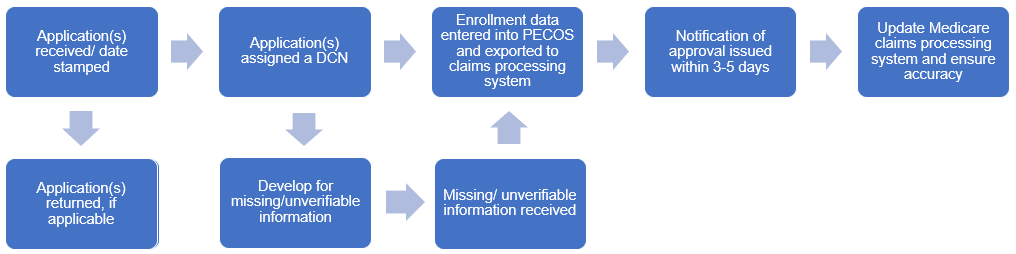
Step 1: Receipt / Initial screening
Applications are:
- Received and date stamped.
- Reviewed for specific criteria, and if applicable, logged and returned to the applicant. A letter will be included indicating the reason for return. Please view Top reasons for immediate returns of enrollment applications article for the return reasons.
- Assigned a document control number (DCN). The Julian date of receipt is embedded in the DCN.
Step 2: Review / Development
CMS requires that all Medicare administrative contractors review each enrollment application in accordance with the Internet Only Manual (IOM) regulations. The regulations that apply to the enrollment process are located in the CMS IOM Pub. 100-08 Medicare Program Integrity Manual, Chapter 10.
During the review process, the provider / supplier may be contacted by a provider enrollment representative to request missing information or to ask for clarification of information (“development”). The additional information will be requested via email, fax, or letter to the contact person provided on the application; the correspondence will provide details related to the information required. Corrections can be faxed or revised via the PECOS. Responses to development must be returned within 30 days from the date of the request. If the requested information is not provided within the allotted timeframe, the application(s) is rejected, and a new application(s) must be submitted to begin the enrollment process again.
To expedite the development process, please provide an email address on your application for either the contact person or correspondence address section of the application. This allows us to email development requests to the appropriate person(s).
Independent diagnostic testing facility (IDTF) only: If you are enrolling as an IDTF, a site inspection will be scheduled after all information is received and validated. The inspection must take place before any further processing occurs. Also, as an IDTF enrollee, the claims processing system will be updated to reflect the specific procedure codes approved for billing, as reported on the CMS-855B application.
Step 3: Data entered into PECOS
Once we have received, reviewed, and approved the enrollment, the information reported on the enrollment application / form(s) is entered into PECOS. During this phase of the process, you may be contacted again to verify information (e.g., real time validations in PECOS may fail causing us to reach out for corrected information; the process cannot continue until the data is corrected). Once all information is entered into PECOS, the information is exported to our claims processing system.
Certified providers / suppliers: If you are enrolling in Part B as a state certified ambulatory surgical center or portable x-ray supplier or if you are enrolling as a Part A provider, we are required to forward your application to the state survey agency / CMS Survey and Operations Group (SOG) Location for final approval.
Step 4: Issuance of notification
You will receive an approval notification letter after your information has been entered into PECOS. This letter will provide you with valuable information regarding the steps you need to take to begin submitting Medicare claims. If an email address was provided on the application, the approval letter will be emailed to the contact person. If no email address was provided on the application, the approval letter will be sent through the mail.
Step 5: Update Medicare processing system
Once all the enrollment information has been exported from PECOS and received in the claims processing system, supplementary information is added to the file to ensure claims process accurately.
Step 6: Finalization
The accuracy of all PECOS / supplementary information is verified in the claims processing system.