Skilled nursing facility (SNF) demand bill
When you, as the skilled nursing facility (SNF), make a determination that a patient does not meet a Medicare skilled level of care upon admission or no longer meets the Medicare skilled level of care at some point during a SNF stay, you must notify the patient or their representative via the SNF Advance Beneficiary Notice of Noncoverage (ABN).
The SNF ABN includes the reason you believe Medicare skilled level of care was not met upon admission or no longer met during the stay, and that you believe Medicare will not pay. This SNF ABN must be signed and dated by the patient or their representative. The date with the signature must reflect the date the patient or their representative was first notified that they do not/no longer meet a skilled level of care.
If a phone call is made to the patient or their representative prior to signing the letter, document your records with the person's name that made the phone call, who they spoke with along with the date and time. Send the letter via 'registered mail' with a return receipt.
For details on the SNF ABN, please review the CMS IOM Pub. 100-04, Claims Processing Manual, Chapter 30, section 70.
If, after receiving notification, the patient or their representative does not agree with your determination, they may request that Medicare process the claim. This is referred to as a demand bill.
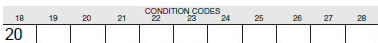
Once they have chosen to request a demand bill, submit the claim with condition code 20 (demand bill) along with all other applicable SNF billing requirements.
Do not submit demand bills for every patient whose care drops below the Medicare skilled level, or for every patient who does not meet the level of care criteria upon admission.
Occasionally, a request for a demand bill is sent at the request of the state where the patient resides for purposes of Medicaid coverage. That review is conducted in the same way as it would be done for a beneficiary requested demand bill.
Submit the demand bill electronically during the regular billing cycle. The claim will suspend for medical review and an additional documentation request (ADR) letter will be sent to you requesting information necessary to complete the demand bill review. The ADR will include the information you need to send and the address to which to send the documentation.
Be sure to include all requested medical records and documents along with a copy of the SNF ABN requesting the review, signed and dated by the beneficiary or their representative (and return receipt if sent via registered mail).
You may not bill the patient until we have completed our review. You may, however, bill for non-covered items, such as TV, telephone, etc.