Medicare secondary payer (MSP): Medicare as the tertiary payer
Medicare providers are expected to determine whether Medicare is the primary or secondary payer before submitting a claim to Medicare. CMS has developed tools, including an MSP questionnaire to help providers identify other payers that may be primary to Medicare.
Refer to the MSP questionnaire in the Medicare Secondary Payer (MSP) Manual, Chapter 3 - MSP provider, physician, and other supplier billing requirements, section 20.2.1 "Admission questions to ask Medicare beneficiaries".
There are times when Medicare becomes the tertiary or third payer. This happens when a beneficiary has more than one primary insurer to Medicare.
Examples:
- A working aged beneficiary who was in an automobile accident
- Beneficiary has two group health plans
It is the primary payer(s) responsibility to pay the claim first. The primary insurers must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit an electronic or paper claim, to Medicare for consideration of secondary benefits or tertiary benefits.
If Medicare is tertiary and only one insurer makes payment, then the claim should be billed with Medicare as the secondary payer. The insurer that did not make payment should not be listed on the claim.
How to properly submit a claim to Medicare for tertiary benefits
Tertiary Claims can be submitted through the Fiscal Intermediary Standard System (FISS) Direct Data Entry (DDE) or by paper utilizing the UB-04 form. At this time, tertiary claims cannot be submitted to First Coast electronically.
To bill paper claims, copies of the primary remittances need to be submitted.
In FISS DDE, the CAS information is entered on the "MSP Payment Information" screen (MAP1719), which is accessible by pressing F11 from Claim Page 03. The "MSP Payment Information" screen for "Primary Payer 1" will display. Entry for a second payer when Medicare is tertiary is available by pressing F6 to display the "MSP Payment Information" screen for "Primary Payer 2." See the screen example below.
FISS DDE MAP1719-MSP payment information
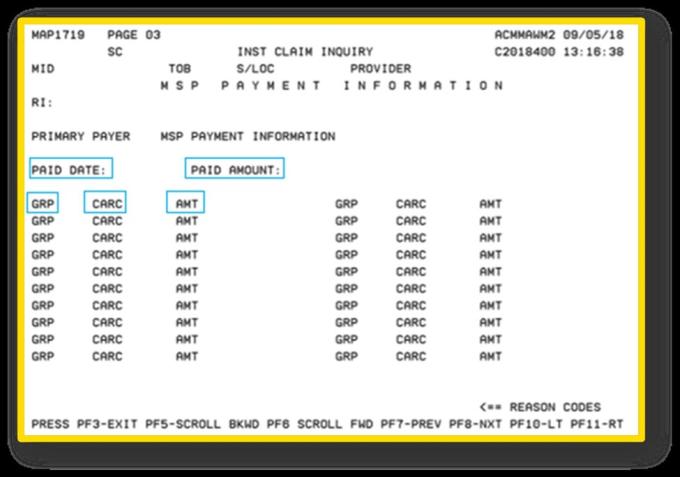
Press F6 to access the "MSP Payment Information" screen for Primary Payer 2 when Medicare is tertiary.
Billing Medicare when both the primary and secondary payer denies the claim
If both the primary payer and the secondary payer deny the claim, a claim is billed to Medicare following the conditional payment process. Only report the occurrence code 24 with the date one of the insurers denied the claim. The claim processing system does not allow more than one occurrence code 24 on a claim. Provide an explanation in the remarks section of the claim.
Tips to ensure accurate MSP claim submissions
- Collect beneficiary health insurance information upon each visit to ensure you have the most current information on file.
- Identify the primary payer(s) prior to submission of a claim and bill the appropriate responsible payer(s) for the related services.
- Use correct diagnosis codes, especially for accident-related claims.
Remember: A properly filed claim prevents First Coast from improperly denying claims and expedites the payment process.
References