Part B service-specific review – clinical laboratory lipid panel (80061)
On August 17, 2020, medical review activity resumed, as directed by CMS, with implementation of post-payment service-specific medical record review.
First Coast is tasked with preventing inappropriate Medicare payments. One of the ways this is conducted is through medical review of claims. This helps to ensure that Medicare pays for services that are covered, coded correctly, and medically reasonable and necessary.
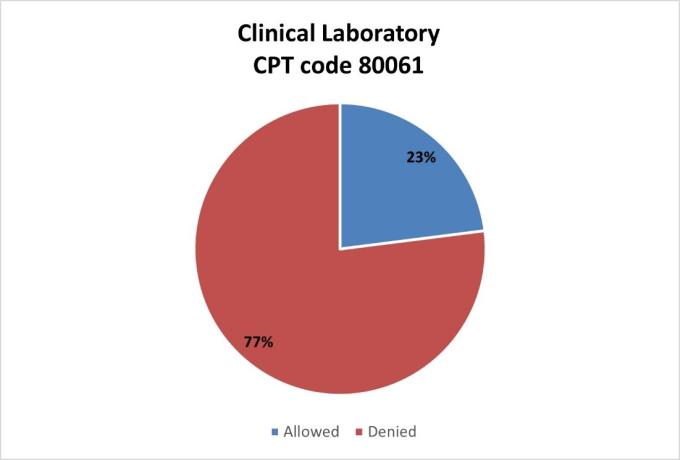
High level results and top denial / partial denial reasons are listed below for the post-payment service specific reviews for lipid panel that have been conducted by First Coast. If you have questions about your individual results, please contact the nurse reviewer assigned to your review for additional information.
Lipid panel (CPT code 80061) (June and July 2021)
Top full / partial denial reasons:
The most common reasons for denial or partial denials are the following:
- Medical necessity – Documentation submitted did not support the service as medically necessary and reasonable.
- The documentation submitted did not support a history and/or treatment that warranted testing.
- The documentation submitted did not support a history and/or treatment that warranted testing.
- Insufficient documentation – The documentation provided was insufficient to support the services as billed to Medicare. First Coast Medical Review makes multiple attempts to correct these error types before completion of the review.