Fast facts: Skilled nursing facility (SNF) helpful hints
The Comprehensive Error Rate Testing (CERT) review contractor (RC) randomly selects a statistically valid sample of Medicare Fee-for-Service (FFS) claims and reviews those claims for payment errors. The CERT program considers any payment that should not have been made or that was paid at an incorrect amount (including both overpayments and underpayments) to be an improper payment.
According to the U.S. Department of Health and Human Services 2024 Medicare Fee-for-Service Supplemental Improper Payment Data, SNF inpatient accounted for $5.6 billion dollars in projected improper payments with an improper payment rate of 17.9%. Insufficient documentation accounted for 75.5% of SNF errors.
In an effort to lower the SNF improper payment rate, we are committed to educating the provider community about proper billing.
For this month’s CERT fast facts, we are sharing some helpful hints to avoid common SNF errors:
- The patient must have a supporting three-day inpatient hospital stay or meet the requirements to waive the three-day qualifying stay.
- The patient must have a need for daily skilled nursing or rehabilitation services:
- Medicare Part A covers Medicare-certified SNF skilled care. Skilled care is nursing or other rehabilitative services, provided according to physician orders, that:
- Require skills of qualified technical or professional health personnel, like:
- Registered nurses
- Licensed practical or vocational nurses
- Physical therapists
- Occupational therapists
- Speech-language pathologists or audiologists
- Skilled nursing or skilled rehabilitation personnel, or others under their general supervision, provide:
- Supervision requiring initial direction and periodic inspection of the actual activity
- Services that an assistant performs when a supervisor isn’t always physically present or at the location
We consider a service skilled if, because of its complexity, you can only perform it safely and effectively by, or under the supervision of, skilled nursing or skilled rehabilitation personnel.
Providers must submit documentation timely upon request from CERT/MAC.
Certifications and recertifications must be completed and signed timely by the physician and submitted upon request. Delayed certifications must provide documentation to support the delay.
All signatures must be legible and meet Medicare signature requirements.
Minimum Data Set (MDS) completion:
- To take credit for an IV, the patient must currently, or within the seven-day look back period, have/had an IV and is receiving medications or fluids intravenously.
- To take credit for Malnutrition, there must be supporting documentation from the physician or physician agreement with the dietician assessment.
- To take credit for shortness of breath while lying flat, the supporting documentation must be in the medical record.
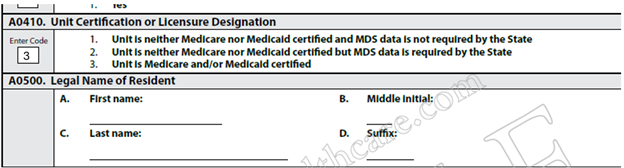
- MDS item A0410: Claim denied as no MDS in the repository because option three was not selected. If option one or two was selected SNF will need to call the state, complete a form, and allow the MDS to be entirely manually deleted. Unable to locate MDS for review until the assessment is completed and submitted again with the correct value code for MDS Item A0410. RAI Manual section 5.8
References