Last Modified: 2/8/2024
Location: FL, PR, USVI
Business: Part A, Part B
Providers may check the status of their
paper or online applications through First Coast’s tool.
Note: Your application status
may not be available until
15 days of the date it is received by First Coast.
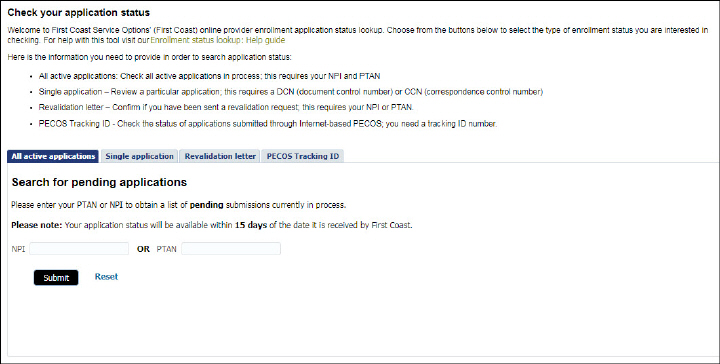
This versatile application allows you to check the status of your enrollment in the Medicare program in four ways:
• You may search for all active/pending applications by entering your NPI or PTAN
• You may check the status of a specific application by entering the nine-digit DCN (document control number) or 12-digit correspondence control number (CCN) and three-digit record number (listed in your acknowledgement letter)
• You may check to determine if you have been sent a revalidation request letter by entering your NPI or PTAN
• You may check on the status of any pending applications by entering the internet-based PECOS Tracking ID.
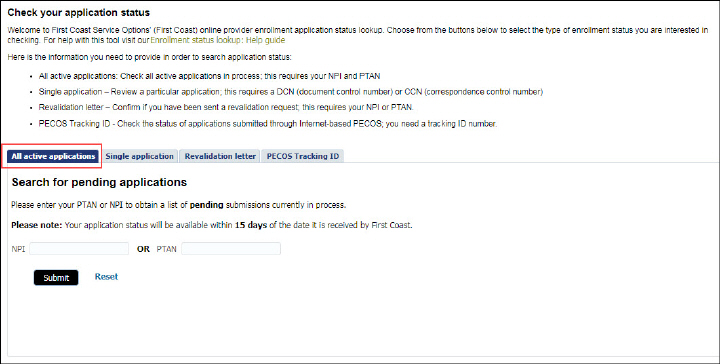
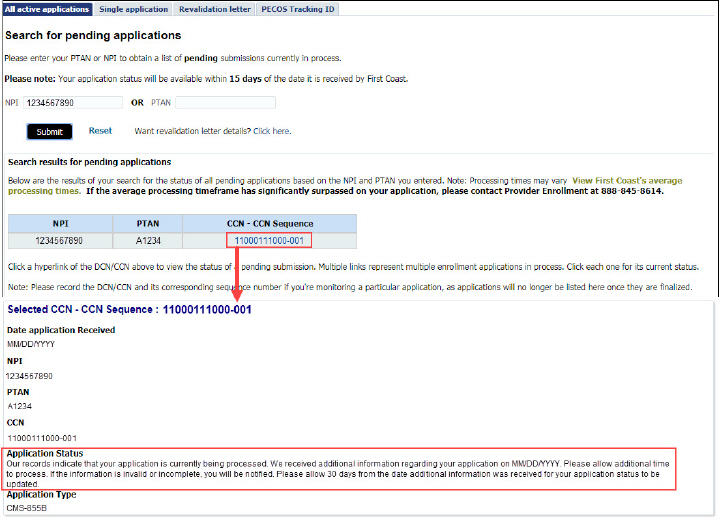
Use this option to check the status of any pending enrollment applications associated with your NPI or PTAN.
1. To search for all pending applications that are currently “in process,” select the All active applications tab (note the tool defaults to this tab upon arriving to the page):
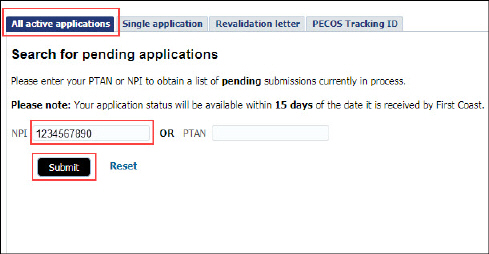
2. Enter your 10-digit NPI (numbers only) and/or enter your six-digit PTAN (numbers and letters)
3. Click the Submit button
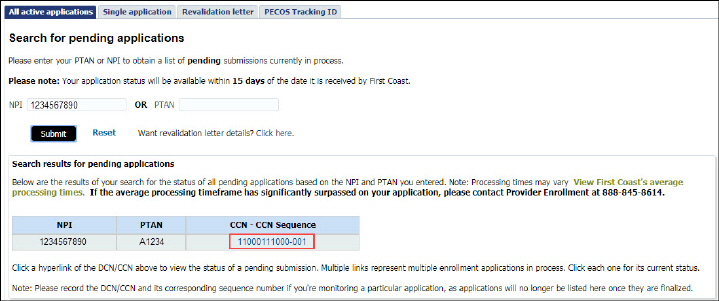
4. The search results will display all pending applications in the system:
5. Click the link to the application you wish to review
6. The application status results will display information associated with the specific application you selected, including its DCN/CCN, receipt date, application type, processing/approval status, and any actions needed to be taken at its current stage in the enrollment process (e.g., timeframe for sending requested information, when to expect an approval letter):
7. Once you have reviewed your results, you may select the link to any other pending applications, or you may initiate a new search by clicking the Reset link.
8. You may also view any revalidation letter details by clicking the revalidation link next to Submit and Reset.
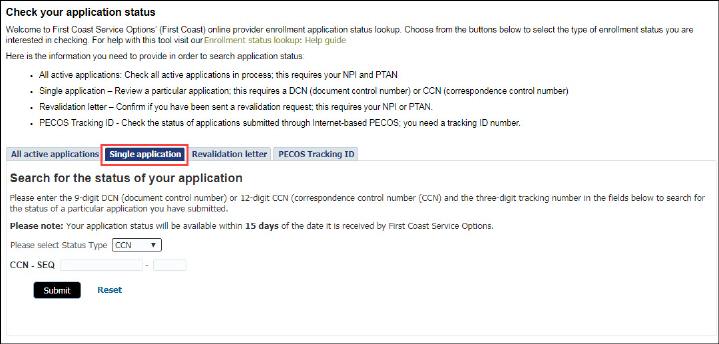
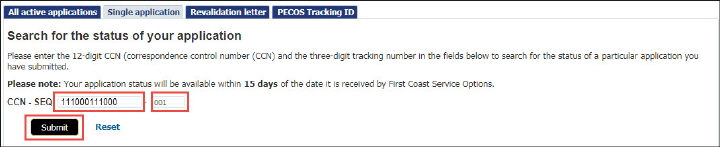
Use this option when you know the nine-digit DCN or the 12-digit CCN and the three-digit record number of a specific application you wish to review.
1. To search for a specific application that is currently “in process,” click the Single application tab:
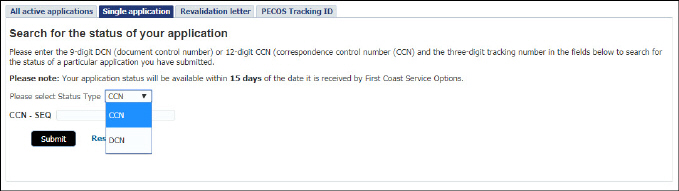
2. Note: The ‘Select Status Type’ currently defaults to search by CCN. Enter the 12-digit CCN and the three-digit record number listed in your acknowledgement letter (numbers only).
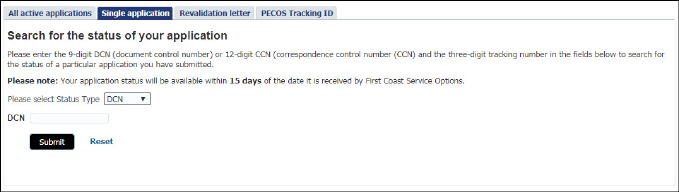
If you have a DCN, please select DCN from the Status Type dropdown and enter the nine-digit DCN listed in your acknowledgement letter.
3. Click the Submit button
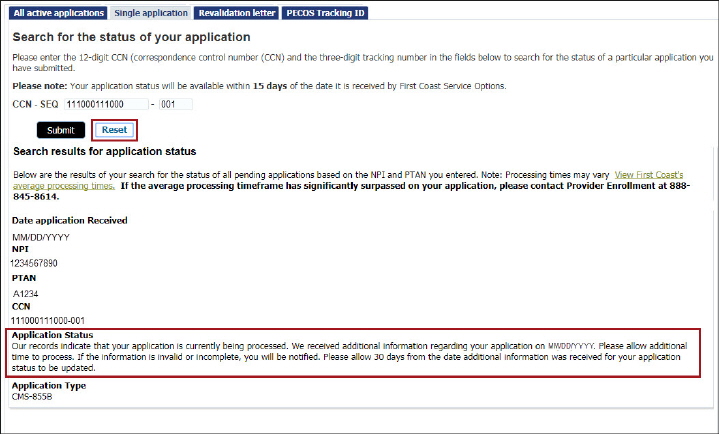
4. The application status results will display information associated with the application, including its DCN/CCN, receipt date, application type, processing/approval status, and any actions needed to be taken at its current stage in the enrollment process (e.g., timeframe for sending requested information, when to expect an approval letter):
5. Once you have reviewed your results, you may initiate a new search by clicking the Reset link.
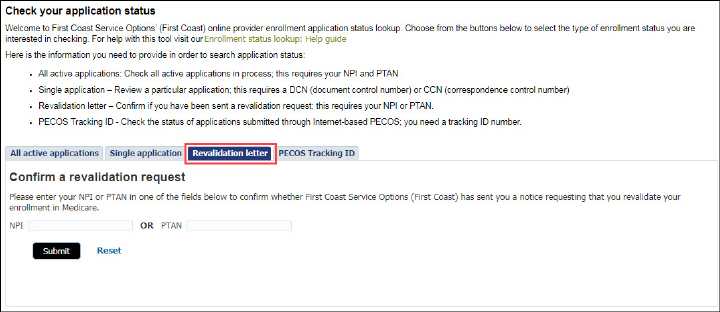
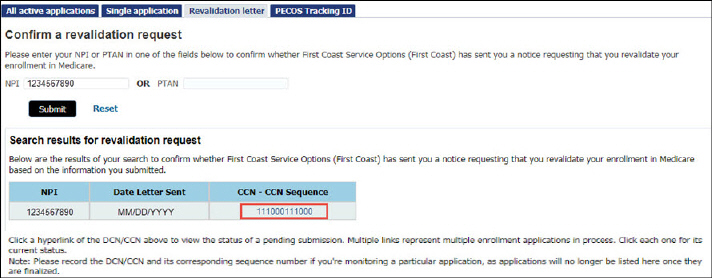
Use this option when you would like to determine whether a revalidation letter has been sent by provider enrollment.
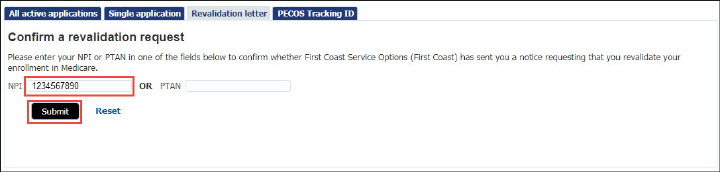
1. To search for a specific application that is currently “in process,” click the Revalidation letter tab:
2. Enter your 10-digit NPI (numbers only) or your six-digit PTAN (numbers and letters)
3. Click the Submit button
4. The revalidation request results will display information associated with any revalidation letters sent to the entity associated with the NPI or PTAN entered. The results will also include the date the revalidation letter was sent and the letter’s DCN/CCN:
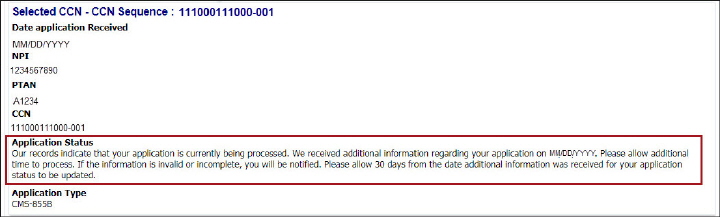
5. Click the DCN/CCN link, and the application status results will display information associated with the application, including its DCN/CCN, receipt date, application type, processing/approval status, and any actions needed to be taken at its current stage in the enrollment process (e.g., timeframe for sending requested information, when to expect an approval letter):
6. Once you have reviewed your results, you may initiate a new search by clicking the Reset link.
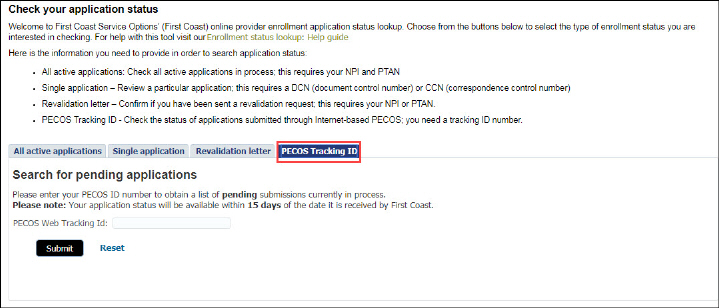
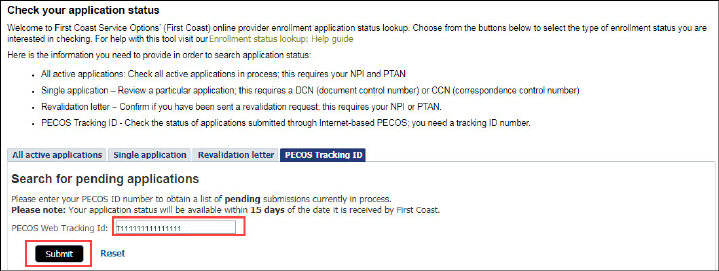
Use this option when you know the Tracking ID associated with one or more pending applications submitted through internet-based PECOS.
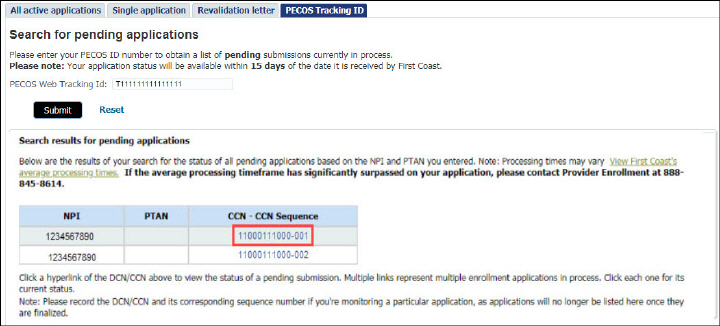
1. To obtain a list of pending submissions that are currently “in process,” click the PECOS Tracking ID tab:
2. Enter the Tracking ID associated with an application submitted through internet-based PECOS
3. Click the Submit button
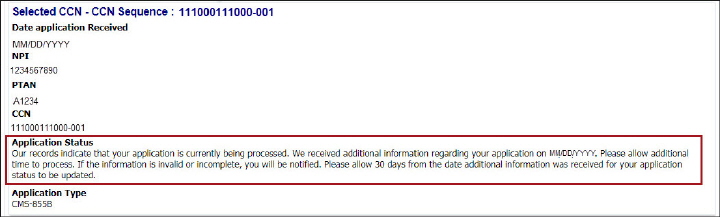
4. The application status results will display information associated with the application, including its DCN/CCN, receipt date, application type, processing/approval status, and any actions needed to be taken at its current stage in the enrollment process (e.g., timeframe for sending requested information, when to expect an approval letter):
5. Click the DCN/CCN link, and the application status results will display information associated with the application, including its DCN/CCN, receipt date, application type, processing/approval status, and any actions needed to be taken at its current stage in the enrollment process (e.g., timeframe for sending requested information, when to expect an approval letter):
You may wish to take advantage of these additional provider enrollment resources:
• Documentation requirements -- encompasses a series of guides that specify qualification requirements and support documentation recommendations. Each guide is focused on a specific provider or supplier type and also includes instructions to address situational-based documentation requirements to furnish proof of resolution of adverse legal actions, proof of identity and authorization to work within the United States, and
Letters of Good Standing for providers located in Puerto Rico.
• First Coast’s eNews subscription page -- subscribe to First Coast's electronic new service and be among the first to learn of the latest Medicare news and other time-critical, essential program information. You will receive regularly scheduled and special enhanced eNews notifications advising you of important changes to Medicare policies as well as the availability of new Medicare publications, informative articles, and upcoming educational events. You can subscribe to one or more lists, ranging from general information to specialties or topics of interest, including provider enrollment.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.



 .
.