Home ►
Help ►
5010 reject code lookup: Help guide
Last Modified: 10/26/2023
Location: FL, PR, USVI
Business: Part A, Part B
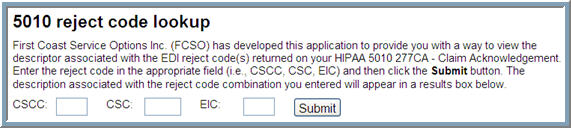
First Coast’s
5010 reject code lookup offers providers the opportunity to resolve data-based issues with their 5010 claim files more quickly by furnishing easy-to-understand descriptions of the reject codes listed in an
STC -- Status information segment of their
277CA -- Claim Acknowledgement.
Users may enter the following information from the STC segment of their 277CA:
• CSCC -- Claim Status Category Code (required): Indicates the general category of the status (e.g., accepted, rejected, additional information requested), which is further detailed in the CSC element.
• CSC -- Claim Status Code (required): Conveys the status of an entire claim or a specific service line.
• EIC -- Entity Identifier Code (when applicable): Unique codes used to identify an entity (e.g., organization, facility, provider, physical location, individual).
1. Verify that your line-of-business (Part A or Part B) has been selected on First Coast’s Medicare provider website
Note: 5010 edit information and associated error code descriptors may vary based upon line-of-business. To change your line-of-business, click the line-of-business link (located underneath the First Coast logo).
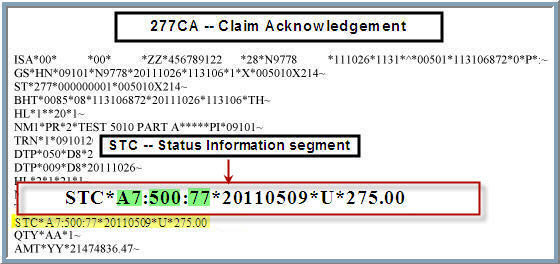
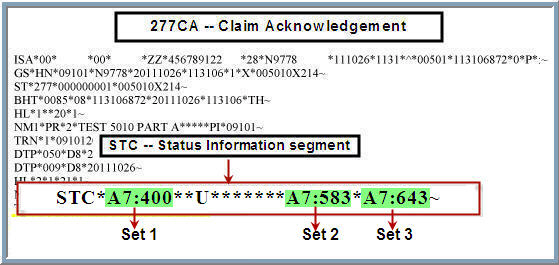
3. Review your 277CA and locate the STC segment
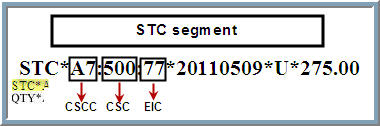
4. Identify reject code data contained within the STC segment
Note: In this example, the STC segment contains CSCC, CSC, and EIC reject code data.
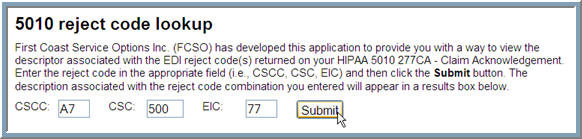
5. Enter available reject code data (i.e., A7, 500, and 77) in the appropriate fields (i.e., CSCC, CSC, EIC) of the 5010 reject code lookup
Note: Although CSCC and CSC are required fields, the EIC field should only be used when EIC data is included within the STC segment. This example includes all three reject codes.
6. Click Submit button
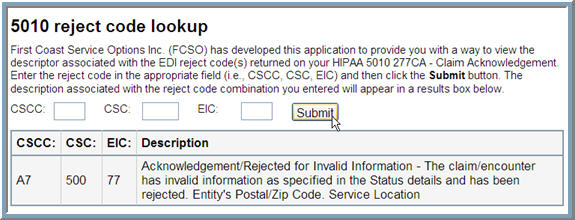
7. Review reject code description
8. Make appropriate adjustments to claim file -- based upon reject code description -- and resubmit to First Coast for adjudication. If you are unable to determine the appropriate action to take to correct the claim, you may call First Coast’s EDI support for additional assistance: 888-670-0940.
Note: In this example, the claim was rejected because the service facility’s postal zip code contained invalid information.
If the STC segment contains multiple sets of CSCC and CSC codes, each set must be entered separately:
1. Verify that your line-of-business (Part A or Part B) has been selected on First Coast’s Medicare provider website
Note: 5010 edit information and associated error code descriptors may vary based upon line-of-business. To change your line-of-business, click the line-of-business link (located underneath the First Coast logo).
3. Review 277CA and locate STC segment
4. Identify each set of CSCC and CSC codes
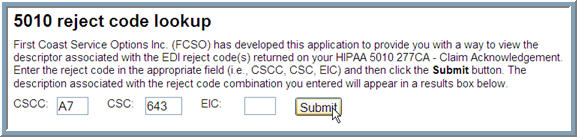
Note: In this example, the STC segment contains three sets of CSCC and CSC reject code data (i.e., A7:400, A7:583, and A7:643). This example does not include EIC data.
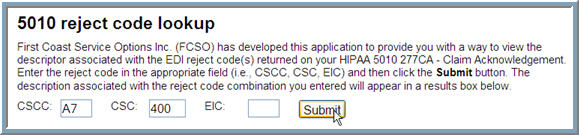
5. Enter first set of CSCC and CSC reject code data (i.e., A7, 400) in the appropriate fields (i.e., CSCC and CSC) of the 5010 reject code lookup
Note: Although CSCC and CSC are required fields, the EIC field should only be used when EIC data is included within the STC segment. This example does not include EIC data.
6. Click Submit button
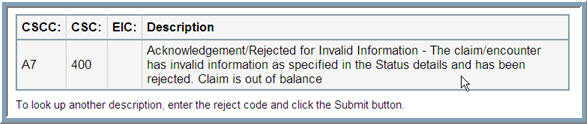
7. Review reject code description of first set
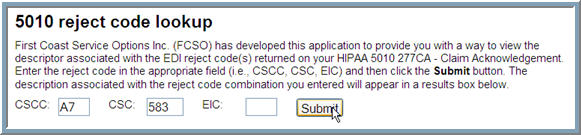
8. Print results page (recommended) and enter second set of CSCC and CSC reject code data (i.e., A7, 583)
Note: Although CSCC and CSC are required fields, the EIC field should only be used when EIC data is included within the STC segment. This example does not include EIC data.
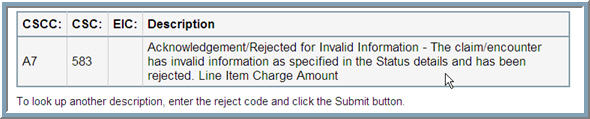
9. Review reject code description of second set
10. Print page (recommended) and enter third set of CSCC and CSC reject code data (i.e., A7, 643)
Note: Although CSCC and CSC are required fields, the EIC field should only be used when EIC data is included within the STC segment. This example does not include EIC data.
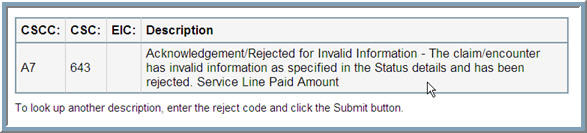
11. Click Submit button
12. Review reject code description of third set
13. Review descriptions of all three CSCC and CSC data sets:
• A7:400: Acknowledgement/Rejected for Invalid Information -- the claim/encounter has invalid information as specified in the Status details and has been rejected. Claim is out of balance.
• A7:583: Acknowledgement/Rejected for Invalid Information -- the claim/encounter has invalid information as specified in the Status details and has been rejected. Line Item Charge Amount.
• A7:643: Acknowledgement/Rejected for Invalid Information -- the claim/encounter has invalid information as specified in the Status details and has been rejected. Service Line Paid Amount.
14. Make appropriate adjustments to claim file -- based upon reject code descriptions from all three data sets -- and resubmit to First Coast for adjudication. If you are unable to determine the appropriate action to take to correct the claim, you may call First Coast’s EDI support for additional assistance: 888-670-0940.
Note: In this example, the claim was rejected because the line item charge amount and the service line paid amount are out of balance and contain invalid information.
For more information, please refer to the following resources:
• HIPAA 5010 implementation guides 
-- ASC X12 offers HIPAA 5010 implementation guides in various formats (downloadable PDF, PDF on CD, bound books, and table data), through its online store.
Note: ASC X12 assists several organizations in the maintenance and distribution of code lists external to the X12 family of standards. The lists are maintained by the Centers for Medicare and Medicaid Services (CMS), the National Uniform Claim Committee (NUCC), and committees that meet during standing X12 meetings.
First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current. Therefore, this is a dynamic site and its content changes daily. It is best to access the site to ensure you have the most current information rather than printing articles or forms that may become obsolete without notice.




 -- ASC X12 offers HIPAA 5010 implementation guides in various formats (downloadable PDF, PDF on CD, bound books, and table data), through its online store.
-- ASC X12 offers HIPAA 5010 implementation guides in various formats (downloadable PDF, PDF on CD, bound books, and table data), through its online store.